
Sugar Addiction: Understanding the Cravings for Sweets
Sugar addiction is a growing concern in today’s food landscape, where sugary snacks and drinks are omnipresent. Many people find themselves grappling with intense sugar cravings, often feeling unable to resist the allure of sweet treats. While the question “is sugar addictive?” is debated among experts, it is evident that the effects of sugar on the brain can lead to compulsive eating behaviors. The health risks of sugar consumption are significant, including weight gain, diabetes, and heart disease, prompting a need for effective sugar consumption tips for healthier eating habits. Understanding the nuances of sugar addiction is crucial in addressing both our relationship with food and our overall health.
When discussing the dependency on sugary foods, terms like ‘sugar dependency’ or ‘sweetness cravings’ often arise. The effects of consuming excessive sweets can mirror those of more recognized addictive substances, leading to discussions about the addictive qualities of sugar and the dangers posed by high sugar diets. Individuals frequently experience powerful urges for sugary foods, akin to the urges seen with alcohol or nicotine, highlighting the psychological and physical dimensions of this phenomenon. While sugar is an essential nutrient found naturally in many foods, distinguishing between necessary intake and overconsumption is vital for maintaining health. Strategies to curb excessive sugar consumption can play a foundational role in breaking the cycle of cravings and fostering a balanced diet.
Understanding Sugar Addiction: A Closer Look
The question of whether sugar is addictive has generated significant debate among nutrition and health experts. While many compare sugar to addictive substances like alcohol or nicotine, the criteria for classifying something as addictive are stringent. Sugar does not fit the classical definition, yet it can cause strong cravings and habitual consumption patterns. This leads to a psychological dependence for some individuals who find it difficult to resist sweet foods. Understanding the mechanisms behind sugar cravings is essential for those looking to reduce their intake.
Research indicates that our modern food landscape contributes to increased sugar consumption, making it challenging to maintain a balanced diet. The prevalence of processed foods loaded with sugar, unhealthy fats, and added sodium keeps cravings at an all-time high. These foods are designed to be hyper-palatable, driving individuals to seek them out repeatedly. So while sugar addiction may not have the same burden of withdrawal as substances like heroin or cocaine, the psychological urge to consume sugary snacks can still lead to negative health outcomes.
The Effects of Sugar: From Cravings to Health Risks
The effects of sugar on our bodies extend beyond just cravings; they can have substantial health implications as well. Chronic high sugar consumption is directly linked to a host of health problems, including obesity, diabetes, and heart disease. These conditions arise not only from the excessive calories consumed but also from the metabolic derangements associated with high sugar intake. Over time, these health risks compound, leading to a significant deterioration in overall well-being.
Moreover, the immediate effects of sugar on mood and energy levels can perpetuate a cycle of cravings—where a temporary spike in energy from sugary foods leads to a subsequent crash, prompting further consumption. This neurological response reinforces the idea that sugar can have addictive qualities, as people may chase that initial high multiple times a day. Understanding these effects is crucial for developing healthy consumption strategies that can minimize the risks associated with high sugar intake.
Tips for Managing Sugar Intake Effectively
Reducing sugar consumption can indeed feel daunting, especially when sweet treats seem so ubiquitous in our diets. However, awareness is the first step toward change. Individuals looking to manage their sugar intake should start by reading food labels meticulously. Many products, even those marketed as healthy, can be deceptively high in added sugars. By learning to recognize hidden sources of sugar, people can make more informed choices about what they consume daily.
Another effective strategy is to gradually reduce sugar in the diet rather than attempting to cut it out completely. Abrupt changes can lead to withdrawal symptoms similar to those experienced when quitting drugs, resulting in rebound cravings. Instead, finding healthier alternatives to satisfy sweet tooth cravings, such as fruit, can help ease the transition. Small, sustainable changes to replace sugary snacks with nutritious options pave the way for long-term success in managing sugar intake.
The Realities of Sugar and Withdrawal Symptoms
While sugar is not classified in the same addictive framework as substances like alcohol or nicotine, withdrawal from habitual sugar consumption can result in real physical symptoms. Individuals who suddenly remove sugar from their diets may experience headaches, mood swings, and fatigue, similar to those encountered when discontinuing certain drugs. These symptoms are primarily due to the body’s adjustment to a drop in sugar levels after having been accustomed to high intakes.
Recognizing these potential withdrawal symptoms can be key to addressing cravings without reverting back to high sugar options. By anticipating these side effects, individuals can prepare themselves mentally and physically, perhaps through supportive nutritional choices, such as increasing fiber and protein intake to maintain energy levels through this transition period.
The Role of Sugar in Our Diet: Finding Balance
Sugar isn’t inherently ‘bad’—in fact, it serves as an important energy source when consumed in moderation. Fruits, for example, provide natural sugars along with vital nutrients and fiber, showcasing that not all sugar is created equal. It’s crucial to distinguish between added sugars found in processed foods and those naturally occurring in whole foods. This understanding can help in building a balanced diet while still enjoying the sweetness that isn’t detrimental to health.
Striking a balance is key; while the average person consumes an excessive amount of added sugar daily, it’s vital to assess personal tolerance. The American Heart Association recommends that men limit their intake to nine teaspoons and women to six. By being mindful of portion sizes and making small adjustments, individuals can bring their sugar consumption in line with health recommendations without feeling deprived.
Cravings: What Triggers Our Desire for Sugar?
Sugar cravings are complex and can be triggered by various factors including emotions, environment, and even physical conditions like low blood sugar. Understanding these triggers can help individuals recognize when they are compelled to reach for sugary foods. Often, emotional states such as stress or sadness can lead individuals to seek comfort in sweets, making psychological awareness an important tool in managing cravings effectively.
In addition, habitual patterns, such as enjoying dessert after meals or having sugary snacks during breaks, can reinforce these cravings over time. Breaking these habits requires both awareness and a concerted effort to replace them with healthier routines, like opting for fruit or nuts. By addressing the underlying triggers, people can better understand their relationship with sugar and work towards moderating their intake.
Exploring the Psychological Effects of Sugar
The psychological impact of sugar extends beyond immediate cravings; it can influence mood and mental health as well. Research indicates that high sugar consumption can lead to mood swings and increased levels of anxiety. For some, this relationship between sugar and mental well-being can create a cycle where individuals consume sugar to self-medicate emotional distress, only to experience negative effects that further compounds the issue.
Becoming aware of how sugar influences psychological states is vital for anyone attempting to reduce their intake. Engaging in mindfulness practices and keeping a journal about moods and sugar consumption can help individuals identify patterns and effects, ultimately aiding in the moderation of sugar intake and promoting healthier coping strategies.
Sugar Classifications: Distinguishing Natural from Added
Understanding the difference between natural and added sugars is an essential component of a healthy diet. Natural sugars, found in fruits, vegetables, and dairy products, come packaged with nutrients that our body needs, facilitating healthy digestion and absorption. In contrast, added sugars, which are often found in processed foods, are devoid of these nutritional benefits and can lead to various health issues when consumed excessively.
Learning how to identify sources of added sugar in foods can empower individuals to make healthier dietary choices. By substituting high-sugar snacks with natural alternatives, individuals can satisfy their sweet cravings while simultaneously nourishing their bodies. Ultimately, this knowledge aids in fostering a healthier relationship with sugar and informs decisions that prioritize overall well-being.
The Social Aspects of Sugar Consumption
Sugar consumption is often imbued with social contexts, as it appears in celebrations, gatherings, and communal eating experiences. Recognizing this can help individuals navigate their sugar intake in a way that balances enjoyment with health considerations. Socializing around foods typically high in sugar can intensify cravings; however, being aware of these dynamics allows individuals to make mindful choices.
Finding joy in shared meals does not have to mean indulging in excessive sugar. Individuals can bring healthier alternatives to gatherings or advocate for better snack options at events, thereby promoting awareness about sugar consumption within their social circles. This encourages a culture of mindful eating and supports others in their journey towards greater health.
Frequently Asked Questions
Is sugar addictive like alcohol and nicotine?
While sugar can enhance cravings and lead to compulsive eating behaviors, it is not classified as an addictive substance like alcohol or nicotine. The physical and psychological effects can mimic addiction, but withdrawal symptoms from sugar are generally less severe. It is important to approach sugar consumption mindfully to prevent excessive intake.
What are the effects of sugar on the brain?
Sugar consumption can activate the brain’s reward system, similar to addictive substances, leading to increased cravings when intake is high. This can create a cycle of habitual consumption as ultra-processed foods often contain added sugars, making them more appealing and difficult to resist.
What health risks are associated with high sugar consumption?
Excessive sugar intake is linked to various health risks, including obesity, type 2 diabetes, heart disease, and dental issues. The American Heart Association recommends limiting added sugar to no more than 9 teaspoons for men and 6 teaspoons for women daily to mitigate these risks.
How can I manage sugar cravings effectively?
To manage sugar cravings, consider gradually reducing sugar intake rather than cutting it out entirely. Incorporating natural sources of sweetness such as fruits, staying hydrated, and consuming balanced meals can help satisfy cravings without resorting to excessive sugar consumption.
What tips can help reduce sugar consumption?
Start by reading food labels to identify hidden sugars, choose whole foods, and limit sugary beverages. Gradually substituting sugary snacks with healthier options like fruits or nuts can also help manage cravings while promoting a balanced diet.
| Key Points |
|---|
| Sugar is associated with cravings and compulsive eating but is not officially classified as an addictive substance like alcohol or nicotine. |
| Ultra-processed foods containing added sugars contribute to increased cravings due to their palatability and convenience. |
| Withdrawal-like symptoms from sugar cessation can occur but are less severe compared to addiction withdrawal from substances like alcohol or drugs. |
| Moderate sugar consumption can be part of a healthy diet since sugar is found in whole foods that are necessary for survival. |
| The average American consumes nearly 20 teaspoons of added sugar daily, exceeding recommended limits; awareness of sugar intake is essential. |
| Gradual reduction of sugar intake is advised over abrupt cessation to avoid potential negative effects on well-being. |
Summary
Sugar addiction is a topic of significant concern as it affects many people’s eating habits and overall health. Although sugar does influence cravings and can lead to habitual consumption, it does not meet the clinical criteria for addiction like alcohol or nicotine. This nuanced understanding emphasizes the importance of moderation and mindful eating rather than categorizing sugar as a strictly addictive substance. By being aware of sugar intake, individuals can enjoy its benefits without falling into the pitfalls of excessive consumption.

Indoor Air Quality: How It Affects Your Health and Focus
Indoor air quality plays a crucial role in our overall health and well-being, impacting everything from our daily comfort to our cognitive function. In modern society, where people spend 80% of their time inside buildings, the quality of the indoor environment has become a primary concern for both individuals and businesses. Poor indoor air quality can exacerbate health issues, leading to reduced productivity and workplace wellness challenges. Researchers, including experts like Joseph Allen from Harvard, emphasize the importance of maintaining clean air within our homes, offices, and schools to promote healthier buildings. Taking proactive measures to improve air quality can drastically enhance our quality of life and significantly reduce health-related complaints.
The atmosphere within enclosed spaces, such as homes and workplaces, can greatly influence our health and overall performance. Terms like indoor environmental quality and breathability describe the conditions that determine how air circulates and is filtered within these spaces. As we increasingly recognize the connection between our surroundings and our health, factors like ventilation rates and pollutant levels become critical in discussions about building design and maintenance. Enhancing the purity of an indoor setting not only fosters a physical sense of comfort but also supports cognitive abilities and mental wellness. By prioritizing clean air, we pave the way for healthier living and thriving environments.
Understanding Indoor Air Quality
Indoor air quality (IAQ) is crucial for maintaining a healthy living and working environment. The air we breathe indoors can contain pollutants such as dust, mold, and volatile organic compounds (VOCs), which can significantly impact our physical health and cognitive function. Research indicates that poor indoor air quality can lead to respiratory issues, reduced concentration, and overall discomfort, ultimately affecting workplace wellness and productivity.
In recent years, experts have emphasized the connection between IAQ and cognitive function. Studies show that enhanced ventilation and cleaning practices can improve air quality, thereby enhancing workers’ focus and reducing fatigue. For instance, workplaces that invest in proper air filtration systems and increase outdoor air circulation report a decrease in employee sick days and an improvement in mood and job satisfaction, leading to healthier buildings overall.
The Impact of Indoor Environments on Health
The design and maintenance of indoor environments profoundly influence our health. Buildings that prioritize health and wellness not only provide fresh air and adequate ventilation but also incorporate materials that minimize harmful emissions. By doing so, they create spaces that promote better physical and mental well-being. The significance of a healthy indoor environment cannot be overstated, as it directly correlates to our ability to thrive in both personal and professional domains.
Moreover, the emphasis on healthy buildings is growing, especially in response to increasing awareness about air quality health. Organizations are actively seeking ways to optimize their indoor environments, recognizing that it impacts employee performance and creativity. By implementing design strategies that include natural light, air purification systems, and eco-friendly materials, companies are leading the charge towards creating healthier workplaces that benefit all occupants.
Improving Workplace Wellness Through Air Quality
Workplace wellness is an essential aspect of any successful organization, and improving indoor air quality plays a critical role in achieving it. Poor air quality can lead to a multitude of health issues such as headaches, fatigue, and drowsiness, which in turn affect productivity. A healthy workplace environment fosters better employee morale and reduces turnover rates, making it a worthwhile investment for organizations.
To create a wellness-focused workplace, employers can take proactive steps like optimizing air ventilation, introducing plants to purify air, and maintaining HVAC systems regularly. Research has shown that simple changes like increasing fresh air intake can elevate cognitive function, leading to a more engaged workforce. These strategies not only contribute to the immediate health of employees but also foster a culture that prioritizes long-term health and sustainable practices.
Enhancing Cognitive Function Through Optimal Air Quality
Cognitive function is influenced significantly by the quality of the air we breathe. Research indicates that environments with superior indoor air quality can enhance cognitive capabilities such as decision-making, problem-solving, and creativity. By ensuring clean, well-ventilated spaces, organizations can empower employees to perform at their best, emphasizing the importance of quality indoor air in bolstering workplace productivity.
Companies are beginning to recognize that investing in indoor air quality leads not only to healthier employees but also to higher overall performance. Implementing rigorous air quality protocols, utilizing advanced air filtration systems, and addressing sources of indoor pollution can promote a more productive work environment. Leaders in workplace wellness understand that the mental prowess of their teams is as vital as physical health, which further justifies the need for comprehensive air quality management.
Creating Healthy Buildings for Optimal Living
The concept of healthy buildings encompasses all aspects of indoor environments, including air quality, lighting, and acoustics. These elements are vital in determining the overall comfort and health of occupants. As more studies reveal the profound effects of our surroundings on health, the construction and renovation of buildings are also increasingly focusing on creating spaces that support well-being.
Healthy buildings not only reduce the risk of health issues but also promote productivity and happiness among occupants. Designers and architects are prioritizing sustainability and health in their projects, using materials that improve indoor air quality and integrating smart technology to monitor air conditions. This shift toward healthier building practices sets a new standard for living and working spaces, ultimately benefiting both individuals and organizations involved.
Air Quality Health and Its Consequences
Air quality health refers to the effects that indoor environments can have on our overall well-being. Pollutants found within homes and workplaces can lead to various health issues, including allergies, respiratory diseases, and even long-term chronic conditions. Understanding how these factors correlate with the quality of air we breathe is essential for promoting healthier lives.
Enhancing air quality should be a priority for everyone, especially in enclosed spaces where pollutants can accumulate. Implementing measures such as regular maintenance of ventilation systems, using air purifiers, and opting for low-VOC materials can significantly improve indoor environments. Prioritizing air quality health is not just about comfort but is vital for preventing health issues and ensuring a better quality of life.
Strategies for Improving Indoor Air Quality
Improving indoor air quality requires a multifaceted approach that considers various factors influencing the air we breathe. Strategies include increasing ventilation rates, utilizing high-efficiency particulate air (HEPA) filters, and conducting regular air quality assessments. These practices can minimize the presence of allergens and toxic pollutants, making indoor environments healthier for all occupants.
Additionally, educating occupants on contributing factors to poor air quality, such as indoor smoking or using certain cleaning products, is crucial. Encouraging practices like using natural products and maintaining humidity levels can dramatically enhance the indoor air environment. The integration of these strategies creates a holistic approach to indoor air quality improvement, fostering healthier and more productive spaces.
The Role of Technology in Enhancing Air Quality
Advancements in technology have revolutionized the way we approach indoor air quality management. Smart sensors and air quality monitors allow for real-time data on pollutant levels, enabling immediate action when air quality deteriorates. Systems can be automated to enhance airflow and filtration based on detected needs, ensuring that indoor environments remain healthy and comfortable.
Moreover, innovations in air purification technology, such as ionization and UV light purification, provide additional layers of protection against airborne contaminants. Embracing these technological solutions empowers individual occupants and organizations to take proactive measures regarding indoor air quality, ultimately leading to healthier buildings and enhanced occupant satisfaction.
Educating for Healthier Indoor Environments
Education plays a crucial role in improving indoor air quality and overall health. It is essential for both employers and employees to understand the direct impacts of indoor air pollutants on health, cognitive function, and productivity. Workshops, informational materials, and regular training sessions can be instrumental in fostering an environment that prioritizes air quality health.
Moreover, as awareness increases regarding the importance of a healthy indoor environment, individuals are more likely to engage in proactive behaviors that sustain good air quality. Communities can benefit from outreach programs that promote clean air practices, ensuring that everyone is equipped with the knowledge to contribute to healthier living and working spaces.
Frequently Asked Questions
How does indoor air quality affect health and cognitive function?
Indoor air quality plays a crucial role in health and cognitive function. Poor air quality, often caused by pollutants like mold, dust, and chemical off-gassing, can lead to health issues such as asthma, allergies, and fatigue. Studies indicate that optimal indoor air quality enhances cognitive function, productivity, and overall workplace wellness.
What are the main sources of indoor air pollution in workplaces?
Common sources of indoor air pollution in workplaces include inadequate ventilation, volatile organic compounds (VOCs) from furnishings, cleaning products, and outdoor air pollutants infiltrating the building. Addressing these sources can improve air quality health and create a healthier indoor environment.
How can I improve indoor air quality in my home or workplace?
To improve indoor air quality, consider increasing ventilation, using air purifiers with HEPA filters, and regularly maintaining HVAC systems. Additionally, using non-toxic cleaning supplies and minimizing clutter can help create a healthier building environment.
What role does ventilation play in indoor air quality and workplace wellness?
Ventilation is vital for maintaining good indoor air quality as it helps dilute and remove indoor pollutants. Enhanced air ventilation has been shown to improve workplace wellness by reducing symptoms like headaches and fatigue, ultimately boosting cognitive performance.
Are there any health risks associated with poor indoor air quality?
Yes, poor indoor air quality can lead to various health risks, including respiratory issues, headaches, and reduced cognitive function. Long-term exposure can exacerbate conditions like asthma and allergies, highlighting the need for healthy buildings that support occupant well-being.
What simple actions can be taken to enhance air quality health indoors?
Simple actions include ensuring proper ventilation, utilizing air purifiers, regularly changing HVAC filters, keeping humidity levels in check, and using houseplants that naturally filter indoor air, all contributing to healthier indoor environments.
How does indoor air quality vary between homes and commercial buildings?
Indoor air quality can vary significantly between homes and commercial buildings due to different ventilation systems, cleaning protocols, and usage patterns. Commercial buildings often experience more foot traffic and varied pollutant sources, necessitating robust indoor air quality management.
Can indoor air quality impact productivity and performance in the workplace?
Absolutely, studies show that poor indoor air quality can negatively impact productivity and cognitive function, leading to decreased performance at work. Improving air quality is essential for ensuring a conducive and healthy workplace environment.
What is the significance of HEPA filters in improving indoor air quality?
HEPA filters are highly effective in trapping airborne particles, including allergens and pollutants, thus significantly improving indoor air quality. Their use in air purifiers and HVAC systems can lead to a healthier indoor environment and enhance air quality health.
How does indoor air quality relate to the concept of healthy buildings?
The concept of healthy buildings focuses on creating environments that promote occupant health through improved indoor air quality, natural lighting, and ergonomic designs. Ensuring good air quality is a foundational aspect of this concept, directly impacting the well-being and productivity of its occupants.
| Question | Answer Choices | Key Point |
|---|---|---|
| 1. How much of their lives do Americans on average spend indoors? | 80%, 65%, 90%, 75% | Americans spend approximately 90% of their lives indoors, emphasizing the importance of indoor air quality. |
| 2. Which workplace change boosted workers’ cognitive function in a 2015 Harvard study? | Switch to open office layout, Building increased air ventilation, Water filters installed in the kitchen | Increased air ventilation has been shown to significantly boost cognitive function in work environments. |
| 3. Building air ventilation rates shifted in the 1970s, with the main goal of: | Reducing asthma attacks, Improving cognitive function, Limiting complaints related to body odors, Preventing transmission of influenza | The shift aimed primarily at improving air quality to limit complaints related to indoor odors. |
| 4. Where do you breathe most outdoor air pollution? | Outdoors, Indoors | Surprisingly, most outdoor pollution is inhaled indoors, underscoring the critical need for better indoor air quality measures. |
| 5. If you live in an apartment, how much of the indoor air is coming from your neighbor’s apartment? | 0%, 1%, 9%, 30% | Up to 30% of the air in an apartment may originate from neighboring units, highlighting air quality concerns in multi-family housing. |
| 6. How many opportunities can you identify to make this building healthier? | 3, 5, More than 10 | Identifying just a few opportunities can lead to significant improvements in overall indoor air quality and health. |
| 7. How much of the air you breathe indoors just came out of the lungs of others in the room? | A considerable amount (up to 3% or more) of indoor air may be exhaled air from others, affecting air quality. | |
| 8. Actions you can take to reduce the spread of infectious diseases indoors: | Bring in more outdoor air, Increase level of filtration, Use portable air cleaners with HEPA filters, All of the above | Implementing multiple strategies can effectively reduce indoor disease transmission risk. |
| 9. Dust is hormonally active. True or False? | True, False | Dust contains hormonally active substances, which can have adverse health effects. |
| 10. Of the 80,000-plus chemicals available for commerce, how many have been banned by the EPA since 1976? | 200, 6, 33 | Only 200 chemicals have been banned since 1976, raising concerns about the safety of many substances in our environment. |
Summary
Indoor air quality is crucial for our overall health and well-being, as it significantly impacts how we feel and function in our daily lives. Awareness of the factors affecting indoor air can empower individuals to take steps, such as improving ventilation and reducing pollutants, to create healthier living and working environments. As evidence suggests a strong link between the quality of the air we breathe indoors and our cognitive abilities, it is essential to prioritize indoor air quality for better health outcomes.

AI in Healthcare: Transforming Patient Care and Medicine
AI in healthcare is revolutionizing the way providers deliver patient care, streamline operations, and make diagnoses. By leveraging advanced artificial intelligence in medicine, healthcare professionals can access vast amounts of data and research in the blink of an eye. Medical AI tools are not just enhancing clinical decision-making but are also significantly improving the efficiency of healthcare technology. The benefits of AI in healthcare are numerous, from reducing administrative burdens to enhancing diagnostic accuracy, ultimately leading to better patient outcomes. As we stand on the brink of this technological evolution, the impact of AI on patient care promises to reshape the landscape of medical practice as we know it.
The integration of artificial intelligence into the medical field is ushering in a new era of innovation that redefines patient interactions and operational efficiency. This shift towards intelligent healthcare solutions includes the deployment of advanced algorithms that empower clinicians with rapid access to critical data. As healthcare systems become increasingly reliant on healthcare technology, the role of AI in enhancing the overall quality of care cannot be understated. With its multifaceted implications, AI’s influence extends to improving decision-making processes and minimizing errors in treatment, showcasing its potential to transform the patient experience in profound ways.
The Revolution of AI in Healthcare
Artificial intelligence in healthcare is not merely a futuristic concept; it is reshaping the landscape of medicine today. With the advent of sophisticated AI tools, healthcare professionals are finding themselves equipped with unprecedented capabilities to analyze data and provide insights. For instance, the use of large language models allows clinicians to access relevant medical literature instantaneously, enhancing decision-making processes in real-time. This leap in technology mirrors significant historical milestones such as the decoding of the human genome, cementing its potential to transform how care is delivered.
Moreover, AI’s transformative impact extends beyond just efficiency in patient care; it fosters better doctor-patient communication. Clinicians equipped with AI tools can engage more meaningfully with patients, leading to improved relationships and care experiences. As healthcare technology evolves, it becomes increasingly clear that leveraging AI in patient interactions can help bridge the gap between clinical expertise and empathetic communication.
AI Benefits in Healthcare Delivery Efficiency
One of the key benefits of implementing AI is its ability to streamline healthcare delivery. By automating routine tasks and reducing paperwork, medical AI tools significantly alleviate administrative burdens that often lead to clinician burnout. For example, ambient documentation systems can capture patient interactions in real-time, allowing physicians to focus on direct patient engagement rather than tedious record-keeping. This not only enhances job satisfaction among healthcare workers but also optimizes patient outcomes by promoting consistent and accurate documentation.
Furthermore, the integration of AI in healthcare can drastically improve the speed and accuracy of diagnoses. Tools powered by artificial intelligence can analyze vast amounts of data, identifying patterns that might be overlooked by human eyes. Studies have suggested that AI-driven diagnostic tools can even outperform seasoned clinicians in certain scenarios, thereby offering a new paradigm for patient diagnoses and care management. As these technologies evolve, healthcare providers will be able to deliver more effective treatments faster than ever before.
The Impact of AI on Patient Care
AI’s growing presence in healthcare has profound implications for patient care, enhancing both diagnostic accuracy and treatment customization. By analyzing data from various sources, including electronic health records and genetic information, AI can help clinicians tailor treatment plans to individual patients’ needs. This results in a more personalized approach to medicine, where the unique characteristics and circumstances of each patient are taken into account, ultimately leading to better health outcomes.
Additionally, AI tools can assist in predicting patient risks and outcomes, allowing healthcare providers to intervene proactively. For instance, algorithms that assess patients’ electronic health records can identify those at higher risk for certain conditions and recommend preventative measures. This shift from reactive to proactive care not only boosts patient satisfaction but also contributes to overall public health improvements, emphasizing the transformative role of AI in delivering superior patient care.
Addressing Bias in AI Systems
While the potential of AI in healthcare is immense, the risk of bias in AI systems raises significant concerns. Many AI algorithms are trained on datasets that may reflect existing inequalities in healthcare, perpetuating disparities in treatment and outcomes. For instance, if data predominantly include cases from affluent populations, the AI’s recommendations may not be applicable to underrepresented groups. This highlights the critical need for careful oversight and diversification in the data used to train these systems.
Furthermore, addressing biases in AI is essential to avoid reinforcing systemic inequities within healthcare. Developers must prioritize inclusive data that represents diverse demographics and medical backgrounds. By doing so, AI applications can be refined to enhance their effectiveness across various populations, ultimately leading to equitable healthcare solutions for all patients.
Training Tomorrow’s Medical Professionals with AI
As AI technology becomes increasingly integrated into clinical practice, its implications for medical education are profound. Future healthcare professionals will need to be adept at working alongside AI tools, which will undoubtedly enhance their training experiences. Incorporating AI into curricula allows students to hone their skills in interpreting data, understanding algorithms, and leveraging AI applications effectively in their practice.
Moreover, employing medical AI tools in educational settings can prompt students to think critically about the information provided by AI systems. This metacognitive approach encourages future physicians to reflect on their decision-making processes and ensures they remain engaged in the ongoing learning journey necessary for effective patient care. Such educational advancements are essential to prepare healthcare students for a future where AI will be an indispensable component of clinical practice.
Ensuring Accuracy and Reliability in AI Applications
As with any transformative technology, ensuring the accuracy and reliability of AI systems is paramount. Instances of AI ‘hallucinations’, or inaccuracies produced by these systems, pose serious risks in medical settings where decisions can have life-or-death consequences. Medical professionals must remain vigilant in scrutinizing AI-generated information and should not rely solely on these tools without critical assessment.
Furthermore, continuous evaluation and iteration of AI systems are necessary to improve their performance. By integrating feedback from clinicians and leveraging real-world experiences, developers can refine algorithms to enhance accuracy. This dedication to ongoing improvement will be crucial in building trust and efficacy among healthcare providers who utilize AI in their daily practice.
AI and the Future of Medical Research
The integration of AI into medical research heralds a new era of innovation and discovery. AI-driven tools can analyze vast datasets quickly, providing insights that would be unfeasible for human researchers alone. This capability not only accelerates the pace of research but also encourages the exploration of previously overlooked areas of study, such as rare diseases or complex biological pathways.
Moreover, AI applications can help identify potential correlations within data that lead to groundbreaking clinical trials and research directions. By synthesizing information from numerous studies, AI can support hypothesis generation, prioritize research resources, and ultimately lead to advancements in treatment and healthcare delivery. This collaborative potential between AI and researchers is essential for enhancing the future of medical science.
Challenges of Adopting AI in Clinical Settings
Despite its transformative promise, the implementation of AI in clinical settings faces several challenges. Resistance from healthcare professionals who are accustomed to traditional methods can impede the acceptance of new technologies. Additionally, the fear of job displacement or reduced human interactions in patient care weighs heavily on many clinicians, complicating the integration process.
To overcome these obstacles, it’s crucial to involve healthcare professionals in AI development and implementation. By focusing on how AI can enhance, not replace, human judgment, stakeholders can foster a collaborative environment that values both technological innovation and the irreplaceable elements of compassionate care. Education and transparency about AI’s role in supporting clinicians will be essential in navigating the evolution of healthcare technology.
The Role of Regulatory Frameworks in AI Governance
As AI applications continue to proliferate in healthcare, establishing robust regulatory frameworks is essential for ensuring patient safety and ethical practice. Regulatory bodies must develop clear guidelines regarding the deployment of AI tools, including standards for data privacy, security, and bias mitigation. The fast-paced nature of AI innovation necessitates that these regulations keep pace with technological advancements to safeguard public health.
Additionally, collaboration between policymakers, healthcare professionals, and technology developers is vital in shaping comprehensive regulations. Open dialogue will help create a regulatory environment that not only facilitates innovation but also prioritizes patient care and equity. Such proactive governance will be essential to navigate the complexities of integrating AI into the healthcare landscape.
Frequently Asked Questions
What are the key benefits of AI in healthcare?
AI in healthcare brings numerous benefits, including improved diagnostic accuracy, enhanced patient care, reduced administrative burdens, and increased efficiency. Medical AI tools utilize advanced algorithms to analyze vast datasets, leading to personalized treatment plans and better patient outcomes. Furthermore, the integration of artificial intelligence in medicine can streamline workflows, allowing healthcare professionals to focus more on direct patient interactions.
How is artificial intelligence transforming patient care?
Artificial intelligence is transforming patient care by providing real-time insights and decision support for healthcare providers. AI can analyze medical histories, predict potential complications, and even suggest treatment options, enabling clinicians to make more informed decisions. This technology enhances the overall patient experience by allowing for quicker diagnoses and more tailored care.
What role do AI tools play in medical education?
AI tools are becoming increasingly significant in medical education by facilitating faster learning and deeper understanding of complex subjects. These tools can provide personalized learning experiences, allowing medical students to engage with real-world cases and scenarios. Ultimately, AI in healthcare education equips future doctors with the skills necessary to leverage technology for improved patient outcomes.
What challenges are associated with the use of AI in healthcare?
Despite its many advantages, the implementation of AI in healthcare faces challenges such as data bias, privacy concerns, and the potential for misinformation. There’s a risk that AI systems may perpetuate existing biases if not properly designed and monitored. Additionally, ensuring the accuracy and reliability of AI-generated information is crucial to mitigate risks to patient safety.
How does AI affect the administrative processes in healthcare?
AI is significantly streamlining administrative processes in healthcare by automating routine tasks such as appointment scheduling, billing, and documentation. By reducing the administrative workload on healthcare professionals, medical AI tools allow them to dedicate more time to direct patient care and improving overall health outcomes.
What is the impact of AI on the doctor-patient relationship?
The incorporation of AI in healthcare is enhancing the doctor-patient relationship by freeing up time for healthcare professionals to focus on meaningful interactions with their patients. With AI handling administrative tasks and providing decision support, clinicians can spend more quality time engaging with patients, thus fostering stronger connections and trust.
Will AI replace healthcare professionals in the future?
AI is not expected to replace healthcare professionals but rather augment their capabilities. While medical AI tools can assist with diagnosis and treatment planning, the human touch in patient care remains irreplaceable. The future of healthcare likely involves collaboration between AI and healthcare providers, enhancing both the efficiency and quality of care.
What does the future hold for AI in healthcare?
The future of AI in healthcare appears promising, with ongoing advancements expected to revolutionize various aspects of the industry. From improving patient care and medical research to enhancing educational practices, AI technology is set to play a pivotal role. As the industry continues to adopt AI tools, the focus will be on harnessing their potential while addressing ethical concerns and ensuring equitable access to benefits.
| Key Points |
|---|
| AI in healthcare aims to reduce human suffering and improve patient care through efficiency and accuracy. |
| Medical professionals like Adam Rodman use AI tools to enhance evidence-based medicine and reduce time spent on research tasks. |
| AI tools can reshape doctor-patient interactions, improve administrative tasks, and support medical education. |
| Concerns include biases in AI algorithms, hallucinations of facts, and the risk of diminishing critical thinking skills in healthcare professionals. |
| AI is expected to complement healthcare professionals rather than replace them. |
Summary
AI in healthcare is transforming the medical landscape by enhancing diagnostic accuracy, streamlining administrative tasks, and fostering better doctor-patient relationships. With its potential to reduce inefficiencies and biases, AI promises to revolutionize not only how care is delivered but also how medical professionals interact with technology and patients. As artificial intelligence continues to evolve, it is paramount that the healthcare system harnesses its capabilities responsibly, addressing issues such as data integrity and accessibility to ensure equitable care for all populations.

Alzheimer’s Early Detection: New Home Testing Method Unveiled
Alzheimer’s early detection is crucial in managing one of the most challenging neurodegenerative diseases of our time. Recent research indicates that olfactory testing Alzheimer’s could serve as a significant early warning tool, revealing cognitive impairment symptoms long before memory problems manifest. Researchers at Mass General Brigham have designed a home test for Alzheimer’s that can help identify those at risk, allowing for timely intervention. By assessing a person’s ability to recognize and remember scents, this innovative smell test Alzheimer’s has the potential to uncover early signs of Alzheimer’s disease in a cost-effective and non-invasive manner. With continued studies, we may finally have a reliable method to monitor and predict cognitive decline, empowering individuals with knowledge well in advance of the disease’s progress.
The early identification of cognitive decline can dramatically reshape the approach to managing conditions like Alzheimer’s disease. Researchers have been exploring various methods, one of which includes an innovative olfactory assessment—an approach that focuses on the sense of smell as a predictor of cognitive health. This method aims not just to highlight cognitive impairment symptoms but also to provide a practical solution that can be executed right at home. With advanced home testing options emerging, such as a simple yet effective smell test, caregivers and health professionals can more efficiently spot early signs of neurodegenerative diseases. The ability to detect risks early on is vital in facilitating timely intervention and thoughtful planning for those affected.
Understanding Alzheimer’s Early Detection through Olfactory Testing
Alzheimer’s early detection is an important focus in the fight against cognitive decline. Annually, numerous studies explore innovative methods to identify individuals at risk. Among these advancements, olfactory testing has emerged as a promising tool. Research indicates that the sense of smell can often decline before other cognitive impairments manifest, making it a vital indicator in detecting Alzheimer’s disease early. Developed by researchers at Mass General Brigham, the olfactory test allows individuals to complete assessments in the comfort of their homes, creating a more accessible means of monitoring cognitive health.
The ability to detect Alzheimer’s disease in its early stages is crucial, as it opens doors for earlier interventions and lifestyle changes that may help slow progression. As participants engage in the olfactory assessments, which involve identifying and remembering various odors, those exhibiting cognitive impairment consistently score lower than their cognitively healthy peers. This trend highlights an essential aspect of cognitive impairment symptoms, as olfactory dysfunction can serve as a non-invasive and straightforward method to hint at underlying neurodegenerative conditions.
Innovations in Home Testing for Cognitive Health
The introduction of home tests for Alzheimer’s disease marks a significant advancement in proactive healthcare. With the rise of technology and telehealth services, individuals can now monitor their cognitive health from the comfort of their homes, allowing for greater convenience. Tools like the Aroma Brain Health Test, developed from rigorous research, empower individuals to take their health into their own hands. This empowerment is especially important for older adults, who may have mobility or access issues when traveling to clinics for evaluations.
Additionally, the implications of a viable home test for Alzheimer’s extend beyond individual monitoring. They create opportunities for routine screening, increasing awareness of cognitive impairment symptoms and reducing stigma around Alzheimer’s disease. As a result, those who score lower on these olfactory tests might be encouraged to seek further medical evaluations, enhancing early detection efforts. Such innovations are critical in facilitating timely interventions that can greatly improve quality of life.
Recognizing Cognitive Impairment Symptoms for Early Intervention
Cognitive impairment symptoms encompass a range of experiences that can signal a decline in mental function. These may include memory loss, difficulties with problem-solving, or challenges in carrying out familiar tasks. Notably, early signs of Alzheimer’s may become apparent through subtle changes in these cognitive functions. As research increasingly highlights the correlation between smell and cognitive decline, identifying these early warning signs becomes imperative for those at risk. Engaging in regular odor discrimination tests can reveal pronounced differences in performance between healthy individuals and those with cognitive concerns.
Identifying these cognitive impairment symptoms early not only facilitates intervention but can also guide lifestyle modifications that promote brain health. Research suggests that cognitive training, social engagement, and nutrition can positively influence cognitive reserve. Therefore, awareness of the signs is critical for individuals and caregivers alike, helping them to navigate early intervention strategies that could slow the effects of Alzheimer’s.
The Role of Smell Tests in Alzheimer’s Research
Smell test Alzheimer’s is a term that denotes the growing focus on olfactory function as an early diagnostic tool for Alzheimer’s disease. Researchers are leveraging this connection to deepen our understanding of the disease’s progression. By tracking how odor recognition and discrimination abilities decline, scientists can establish patterns that contribute to diagnosing Alzheimer’s and other neurodegenerative diseases. The ability to conduct these tests at home adds an exciting element to this research, opening new pathways for large-scale studies across diverse populations.
Further developments in odor identification tests could pave the way for comprehensive cognitive evaluations. Studies show that age-related olfactory decline occurs alongside cognitive changes, reinforcing the idea that smell tests are integral to Alzheimer’s research. As tools like the Aroma Brain Health Test advance, they may broaden our knowledge of cognitive impairment and its neurodegenerative counterparts, ultimately guiding future clinical practices and treatment approaches.
Promoting Awareness of Early Signs of Alzheimer’s
Raising awareness about the early signs of Alzheimer’s is crucial for timely intervention and support. Many individuals and families remain unaware of the subtle changes in memory and cognition that can point to the onset of Alzheimer’s disease. By educating the public about symptoms such as frequent forgetting, misplacing items, and having trouble concentrating, we empower individuals to recognize these signs sooner. Increased awareness can lead to earlier testing and intervention, possibly altering the disease’s trajectory. Moreover, connecting symptoms to specific testing, such as olfactory tests, can further enhance recognition.
Community outreach initiatives and education programs focusing on the early signs of Alzheimer’s can have transformative effects. Consideration of olfactory dysfunction, alongside other cognitive impairment symptoms, can enhance the understanding of the disease. Workshops that offer resources, provide access to home tests for Alzheimer’s, and emphasize support networks can encourage more people to proactively assess their cognitive health. As communities become more informed about Alzheimer’s, the stigma surrounding memory loss may diminish, allowing for open discussions and stronger support systems.
The Future of Alzheimer’s Prevention and Management
As our understanding of Alzheimer’s disease evolves, so does the landscape of prevention and management. Early detection, particularly through innovative methods like olfactory testing, holds promise for changing how we approach cognitive health. The National Institutes of Health and other organizations are increasingly recognizing the importance of multifaceted strategies that combine education, testing, and intervention for those at risk. This integrated approach may not only improve individual outcomes but can also influence public health policies aimed at tackling Alzheimer’s as a national concern.
With ongoing research and innovative testing becoming available, the future of Alzheimer’s prevention appears more hopeful. By incorporating olfactory assessments into regular cognitive health evaluations, we can facilitate earlier interventions, which may significantly slow cognitive decline. Additionally, increased momentum towards understanding risk factors, including lifestyle choices, can yield practical recommendations. Ultimately, a proactive approach to Alzheimer’s through testing and education can ensure that individuals are better equipped to manage their cognitive health.
Cultural Considerations in Olfactory Testing
When developing home tests for Alzheimer’s, it’s essential to consider the cultural aspects of olfactory perception. Different cultures may have unique relationships with sensory experiences and might interpret or respond to smell differently. Researchers are ensuring that odor identification tests are effective across diverse populations by including multiple languages and varying olfactory stimuli that resonate with different cultural backgrounds. This culturally sensitive approach increases participation rates and can yield richer data, enhancing our understanding of Alzheimer’s risks.
Incorporating cultural considerations into cognitive health studies supports inclusivity and offers a more comprehensive view of cognitive impairment symptoms globally. By examining how different populations experience smell and memory, scientists can tailor interventions that resonate more closely with specific communities. Furthermore, this attention to cultural differences also lowers barriers to participation, making it easier for individuals from varied backgrounds to engage with their cognitive health proactively.
Empowering Caregivers with Knowledge and Tools
Caregivers play a pivotal role in the management of Alzheimer’s disease, often being the first to notice subtle changes in their loved one’s behavior and cognition. Providing them with knowledge about cognitive impairment symptoms, including early signs of Alzheimer’s, is crucial. Empowerment can begin with resources that explain olfactory testing and its significance in early detection. Understanding the connection between smell and cognitive health allows caregivers to advocate for appropriate assessments and interventions.
Furthermore, supporting caregivers with tools and strategies enhances their ability to provide effective care. Workshops, online courses, and community support groups can bolster their skillset regarding memory care and communication strategies. By equipping caregivers with resources related to Alzheimer’s management, we not only benefit the care recipient but also improve the caregiver’s overall emotional and mental well-being.
The Intersection of Technology and Alzheimer’s Testing
The intersection of technology and Alzheimer’s testing offers promising advancements in cognitive health monitoring. Digital platforms and mobile applications now allow individuals to engage in self-assessments, including olfactory testing, while tracking their cognitive performance over time. These innovations are making it easier for users to identify early signs of cognitive decline in a user-friendly format, encouraging more home-based evaluations and timely interventions.
Additionally, technological innovations pave the way for enhanced data collection and analysis, ultimately informing ongoing research into Alzheimer’s disease. With the incorporation of big data analytics, researchers can uncover patterns and potential risk factors attributable to cognitive impairment symptoms. This synergistic relationship not only improves individual assessments but also aids in the broader understanding of Alzheimer’s disease dynamics and the effectiveness of preventative measures.
Frequently Asked Questions
What is olfactory testing for Alzheimer’s and how does it work?
Olfactory testing for Alzheimer’s involves assessing an individual’s ability to identify and remember different odors. This form of testing has been developed as a part of early detection for cognitive impairment. It allows researchers to identify potential early signs of Alzheimer’s by evaluating smell memory and discrimination, which may indicate the risk of developing Alzheimer’s disease.
Can I perform a home test for Alzheimer’s to check for early signs of cognitive impairment?
Yes, researchers have developed at-home tests for Alzheimer’s that can help individuals assess their risk of cognitive impairment. These tests often involve olfactory tasks where participants smell and identify various scents. Such tests are designed to be simple and non-invasive, making them accessible for early detection of potential Alzheimer’s symptoms.
What are the common cognitive impairment symptoms associated with early signs of Alzheimer’s?
Common cognitive impairment symptoms that may indicate early signs of Alzheimer’s include memory loss, difficulty focusing, trouble with problem-solving, and changes in smell ability. Research suggests that a subtle decline in the ability to identify and remember odors may be an early warning sign for Alzheimer’s disease.
What are the early signs of Alzheimer’s that can be detected through smell tests?
Early signs of Alzheimer’s that can be detected through smell tests include impaired odor identification and decreased smell memory. Studies have shown that older adults experiencing these declines may have an increased risk of developing Alzheimer’s cognitive symptoms in the future.
How effective is olfactory testing in early detection of Alzheimer’s disease?
Olfactory testing has shown promising effectiveness in early detection of Alzheimer’s disease. Research indicates that participants with cognitive impairment score lower on these tests compared to cognitively normal individuals, suggesting that olfactory dysfunction may be a reliable early indicator for Alzheimer’s.
| Key Point | Description |
|---|---|
| Olfactory Tests | At-home tests developed to assess smell discrimination, identification, and memory. |
| Cognitive Impairment | Older adults with cognitive impairment scored lower on olfactory tests compared to cognitively normal individuals. |
| Study Goals | To create a cost-effective, noninvasive at-home test for early Alzheimer’s detection. |
| Participants | Included English- and Spanish-speaking individuals with cognitive complaints and mild cognitive impairment. |
| Potential Applications | Results could pave the way for further research on neurodegenerative diseases and clinical symptom prediction. |
Summary
Alzheimer’s early detection plays a critical role in addressing the disease effectively. The innovative olfactory test developed by researchers allows for identifying individuals at risk of Alzheimer’s years before any symptoms surface. By fostering early intervention and continuous research, this approach marks a significant step forward in understanding and potentially mitigating the effects of Alzheimer’s disease.

Chemical Hazards: Protecting Health with ChemFORWARD’s Database
Chemical hazards pose significant risks to both human health and the environment, permeating our everyday lives through the industrial chemicals found in common products. From the glue in our shoes to the preservatives in our food, awareness of these dangers is essential for public health and environmental safety. Organizations like ChemFORWARD are leading the charge by providing comprehensive toxicity assessments that help businesses understand and mitigate these risks. By systematically analyzing the potential hazards of various substances, ChemFORWARD supports companies in choosing safer alternatives, ultimately striving for a healthier future. As we navigate a world dominated by chemicals, recognizing and addressing chemical hazards becomes increasingly important for ensuring our well-being and protecting our planet.
The intricacies of chemical danger, often referred to as toxic risks or hazardous materials, highlight the need for thorough scrutiny in product manufacturing and safety protocols. The presence of these substances in both consumer goods and industrial applications warrants a cautious approach to public health and environmental integrity. Alternative terminology such as hazardous substances or toxicological risks helps encapsulate the broader spectrum of concerns associated with chemical use. Initiatives similar to ChemFORWARD’s database emphasize the importance of rigorous evaluations and informed decision-making in order to safeguard both the population and the ecosystem. Understanding these alternative terms allows us to deepen our engagement with the issues surrounding chemical safety and its implications for modern life.
Understanding Chemical Hazards in Everyday Products
Chemical hazards are an unavoidable reality in our modern lives, considering the myriad of synthetic substances used in manufacturing products we encounter daily. From clothing to electronics, the presence of industrial chemicals often goes unchecked, leading to potential health risks for consumers. For instance, many textiles contain harmful agents that can contribute to skin irritations and other health complications. Recognizing these hazards is crucial for making informed choices in our purchases.
Organizations like ChemFORWARD are taking significant steps to assess and categorize these hazards. They compile verified chemical hazard assessments that provide crucial information on the effects of various chemicals on human health and the environment. This transparency empowers consumers and manufacturers to prioritize safety and environmental responsibility, ultimately striving for products that are less harmful to both individuals and the planet.
The Role of ChemFORWARD in Promoting Public Health
ChemFORWARD plays a pivotal role in advancing public health by establishing a comprehensive database of chemical assessments. By providing access to toxicity data and minimizing the risks associated with industrial chemicals, it supports companies in making safer product choices. This initiative is essential as current regulations often lack stringent requirements for chemical safety evaluations, allowing potentially dangerous substances to enter the market unchecked.
In conversation with industry leaders, it has become clear that collaboration is key to driving change. Companies partnering with ChemFORWARD, like Google, acknowledge that shared knowledge about chemical hazards can lead to industry-wide advancements in safety standards. By working together, these companies can harness collective insights to improve their product formulations, thereby safeguarding public health and enhancing environmental safety.
Assessing Toxicity: A Comprehensive Approach
Toxicity assessments are critical in identifying the potential risks associated with industrial chemicals. ChemFORWARD utilizes a methodology that evaluates multiple health endpoints, including carcinogenicity and reproductive toxicity, providing a holistic view of a chemical’s safety profile. This rigorous approach ensures that both manufacturers and consumers are equipped with essential information to mitigate health risks associated with chemical exposure.
Moreover, understanding the environmental impact of chemicals is just as important. ChemFORWARD assesses environmental persistence and degradation rates to gauge how substances will affect ecosystems over time. This dual focus on human health and environmental safety promotes a balanced view of chemical use, fostering a culture of responsibility and awareness among businesses and consumers alike.
Environmental Safety: Ensuring a Sustainable Future
Environmental safety is intricately linked to the chemicals we use in everyday products. As awareness about the ecological consequences of industrial chemicals grows, it becomes increasingly important to prioritize sustainable practices. Organizations such as ChemFORWARD advocate for the responsible use of chemicals and the adoption of safer alternatives that do not compromise environmental integrity.
The collaboration of various sectors, including government, business, and academia, is vital for enhancing environmental safety. By sharing data and resources, these stakeholders can work towards establishing regulations that protect ecosystems while also promoting innovations in greener chemistry and sustainable product design.
The Importance of Data Sharing in Chemical Management
Data sharing is an essential component of effective chemical management. Through platforms like ChemFORWARD, vital information about chemical hazards and toxicity assessments can be made accessible to all stakeholders involved in product manufacturing and safety. This cooperation fosters an environment where companies can learn from one another and build on existing research to improve safety standards across industries.
In today’s interconnected world, not sharing information can lead to significant oversights regarding product safety. For example, if one company discovers a chemical’s adverse effects but fails to disseminate that information, others may continue using that hazardous substance unknowingly. Developing a culture of transparency and collaboration is therefore crucial for achieving a safer marketplace.
Innovative Approaches to Chemical Safety
Innovative approaches to chemical safety are paramount as we navigate the complexities of modern manufacturing. ChemFORWARD’s database not only provides historical data about chemical hazards but also encourages forward-thinking solutions that can be integrated into current production methods. This not only protects consumers but also promotes corporate responsibility and sustainability.
As technology advances, new methodologies for chemical assessment and management are also emerging, allowing for real-time data integration and reporting. This enables companies to adapt promptly to evolving safety standards and consumer expectations, ultimately leading to innovative products that prioritize health and environmental safety.
Challenges in Chemical Regulation and Safety
Despite the advancements made by organizations like ChemFORWARD, significant challenges remain in the landscape of chemical regulation and safety. The absence of universal requirements across industries means that many chemicals can still be used without adequate vetting, which poses a risk to public health. Addressing this issue requires comprehensive legislation that mandates thorough assessments of chemical substances before they enter the market.
Moreover, the global nature of manufacturing complicates regulatory efforts further. Different countries have varying standards and practices when it comes to chemical safety, making it difficult to ensure consistent protection for consumers worldwide. Collaborative efforts among international regulatory bodies are essential to establish unified protocols that enhance chemical safety on a global scale.
The Future of Safer Chemistry
The future of safer chemistry looks promising, thanks to initiatives led by ChemFORWARD and similar organizations. By emphasizing the importance of chemical hazard assessments and transparent data sharing, there is a growing movement towards safer manufacturing practices. As consumers become more informed and demand safer products, businesses will be compelled to adapt and prioritize health and environmental safety.
Additionally, continuous advancements in science and technology will facilitate the development of safer alternatives to hazardous substances. Ultimately, the integration of safer chemistry principles into everyday products ensures a healthier future for the planet and its inhabitants.
Collaborative Efforts Across Industries
Collaboration across industries is crucial for advancing safety and sustainability in chemical management. By forming partnerships, organizations can pool resources, share insights, and collectively address challenges related to chemical hazards. ChemFORWARD exemplifies this collaborative spirit by uniting businesses, researchers, and regulators, fostering a holistic approach to chemical safety.
Innovative collaborations can also lead to the development of best practices and shared frameworks for assessing chemical safety. These alliances create opportunities for continual improvement and the establishment of standards that prioritize public health and environmental protection across various sectors.
Frequently Asked Questions
What are chemical hazards and how do they impact public health?
Chemical hazards refer to substances that can cause harm to human health and the environment. They can originate from industrial chemicals used in various products, leading to potential health issues, such as respiratory problems, skin irritations, or long-term effects like cancer. Understanding chemical hazards is crucial for protecting public health, especially as we encounter many chemicals daily in our homes and workplaces.
How does ChemFORWARD contribute to reducing chemical hazards?
ChemFORWARD plays a significant role in reducing chemical hazards by maintaining a database of verified chemical hazard assessments (CHAs). This database helps companies identify the potential risks associated with various industrial chemicals, allowing them to make informed decisions that safeguard public health and promote environmental safety. Their assessments cover multiple health endpoints, aiding in toxicity assessments relevant to compliance and safety standards.
What is the significance of toxicity assessments in industrial chemicals?
Toxicity assessments are critical evaluations that determine the poisonous effects of industrial chemicals on human health and the environment. These assessments help categorize chemical hazards, guiding industries in selecting safer alternatives and minimizing health risks. By understanding the toxicity profiles of chemicals, businesses can enhance their product safety and adhere to regulations aimed at protecting public health.
How can consumers protect themselves from chemical hazards in everyday products?
Consumers can protect themselves from chemical hazards by being informed about the products they use, particularly those containing industrial chemicals. Checking for certifications, seeking out brands committed to transparency, and using resources like ChemFORWARD’s database can help identify safer options. Additionally, being aware of labeling and choosing products with less toxic ingredients significantly reduces exposure to harmful chemicals.
What role does environmental safety play in managing chemical hazards?
Environmental safety is integral to managing chemical hazards as it involves preventing harmful substances from contaminating air, water, and soil. Effective regulation and ongoing checks of industrial chemicals help mitigate risks to both ecosystems and public health. Companies that adopt stringent environmental safety practices improve their overall impact, safeguarding communities from the adverse effects of chemical hazards.
How do industrial chemicals contribute to environmental health issues?
Industrial chemicals can contribute to various environmental health issues by contaminating natural resources, affecting wildlife, and disrupting ecosystems. Persistent chemicals may linger in the environment, leading to bioaccumulation and toxicity at higher levels of the food chain. Consequently, the management and assessment of chemical hazards are essential for preserving ecological integrity and promoting long-term environmental health.
Why is it important to vet industrial chemicals before use?
Vetting industrial chemicals before use is crucial to ensure they do not pose risks to human health or the environment. Effective evaluation, such as through chemical hazard assessments, helps identify potential toxic effects and guides industries in choosing safer alternatives. This proactive approach minimizes exposure to harmful substances, thereby protecting public health and fostering a sustainable manufacturing framework.
What challenges do companies face when assessing chemical hazards?
Companies often face challenges in assessing chemical hazards, including the lack of standardized testing requirements across industries and difficulties in tracking numerous chemicals within their supply chains. Inconsistent data availability and varying regulations complicate the process of ensuring product safety. Collaborations with organizations like ChemFORWARD help address these challenges by providing accessible, comprehensive chemical hazard assessments.
| Key Points | Details |
|---|---|
| Overview of ChemFORWARD | ChemFORWARD is a Washington D.C.-based organization that compiles a database to protect human and environmental health by assessing industrial chemicals. |
| Mission | To make products safer by providing verified chemical hazard assessments (CHAs) for companies in their supply chains. |
| Health Risks | Recognizes that thousands of chemicals are present in everyday items, which can harm health and the planet. |
| Assessment Criteria | ChemFORWARD evaluates chemicals on toxicity and health endpoints such as carcinogenicity, reproductive toxicity, and environmental persistence. |
| Collaboration Importance | Companies gain access to shared chemical assessments, creating a scalable impact on health and safety in various industries. |
Summary
Chemical hazards are a critical concern in modern society, as numerous chemicals used in everyday products can pose health risks to individuals and the environment. Organizations like ChemFORWARD are pivotal in assessing these risks, offering a comprehensive database that helps businesses evaluate and mitigate the dangers linked to industrial chemicals. By promoting a collaborative approach to chemical safety, ChemFORWARD not only enhances product safety but also drives initiatives for healthier public and environmental health.
Exercise Benefits for Colon Cancer Survivors: Live Longer
Exercise benefits for colon cancer survivors are profound, as recent studies reveal that regular physical activity significantly enhances long-term survival rates for patients who have undergone colon cancer treatment. Engaging in consistent workouts not only aids in recovery but also helps narrow the survival gap between these survivors and the general population. Research conducted by Dana-Farber Cancer Institute indicates that patients with stage 3 colon cancer who embrace an active lifestyle experience improved survival rates compared to their less active counterparts. With colon cancer being a prevalent cause of cancer-related mortality, understanding the health benefits of exercise becomes crucial for those striving to enhance their quality of life post-diagnosis. Therefore, incorporating physical activity and cancer recovery strategies into daily routines is essential for maximizing outcomes and fostering longevity for colon cancer survivors.
The advantages of physical exercise for individuals recovering from colorectal cancer are not only scientifically substantiated but also essential for improving overall well-being. Post-cancer treatment, engaging in various forms of physical activity helps to bolster resilience and can significantly impact long-term outcomes, effectively bridging the gap in survival rates. This correlation between exercise and cancer recovery underscores the necessity for survivors to commit to an active lifestyle for better health outcomes. Studies show that maintaining a consistent regimen of physical exertion can lead to a decrease in the risks associated with cancer recurrence, while also contributing to a healthier life post-treatment. Thus, embracing physical activity emerges as a key aspect for those navigating the journey of survival after a diagnosis of colon cancer.
Understanding Colon Cancer Treatment and Recovery
Colon cancer treatment often involves a combination of surgery, chemotherapy, and ongoing monitoring. For survivors, recovery does not solely hinge on medical interventions; lifestyle factors such as nutrition and exercise play a pivotal role. Post-treatment recovery can be an arduous journey, but physical activity positively influences both mental and physical health. Engaging in regular exercise can help mitigate treatment side effects, such as fatigue and depression, thus facilitating a smoother transition back to daily life.
Research continues to shed light on the profound benefits of physical activity during recovery from colon cancer. Beyond physical improvements, exercise fosters a sense of agency among survivors, enabling them to reclaim control over their health. Simple activities, from walking to more structured exercise programs, empower individuals, contributing to overall well-being and vitality post-cancer treatment.
The Importance of Exercise for Colon Cancer Survivors
Exercise has been shown to deliver numerous health benefits for colon cancer survivors, significantly impacting their overall quality of life. A study from the Dana-Farber Cancer Institute revealed that regular physical activity can improve long-term survival rates for stage 3 colon cancer patients, narrowing the survival gap between these individuals and the general population. With physical activity linked to reduced risks of cancer recurrence, the importance of maintaining a regular exercise routine cannot be overstated.
Additionally, survivors who engage in regular exercise display improved psychological well-being. The mental health benefits of physical activity include reduced anxiety and depression levels, providing a holistic approach to recovery that encompasses both body and mind. Encouraging cancer survivors to incorporate exercise into their daily routines can lead to a substantial enhancement in their life satisfaction and emotional stability.
The Connection Between Physical Activity and Cancer Recovery
Evidence supporting the connection between physical activity and cancer recovery continues to grow. Studies highlight how survivors of colon cancer who participate in a consistent exercise regimen experience improved health outcomes compared to those who lead sedentary lifestyles. One significant finding suggests that survivors engaging in higher levels of physical activity demonstrate survival rates similar to the general population, emphasizing the role exercise plays in recovery.
Moreover, physical activity during recovery can be integral to combating treatment side effects. Weight gain, loss of muscle mass, and fatigue are common post-treatment challenges faced by survivors. Incorporating moderate-intensity activities into their daily lives helps mitigate these effects, enhancing physical fitness and health resilience. Ultimately, exercise serves as a powerful ally in the recovery journey for colon cancer survivors.
Health Benefits of Exercise for Cancer Patients
The health benefits of exercise extend far beyond physical improvements, especially for cancer patients. Regular activity can bolster the immune system, enhance cardiovascular health, and help maintain a healthy weight—critical factors for colon cancer survivors. By engaging in moderate exercise, these individuals can significantly reduce the risk of developing comorbid conditions associated with poor health outcomes post-treatment.
Additionally, exercise can serve as a psychological boost, helping cancer survivors combat feelings of isolation and stress often experienced during recovery. Group exercises or community classes can provide social support alongside physical benefits, creating a multifaceted approach to health enhancement. Research illustrates that patients who prioritize exercise not only improve their physical condition but also cultivate resilience and optimism during a challenging recovery phase.
Addressing Long-Term Survival in Colon Cancer Patients
Long-term survival after colon cancer treatment is a common concern for many patients. Engaging in regular exercise has been linked to improved long-term survival outcomes, with studies indicating that survivors who maintain an active lifestyle have much better prospects than their less active counterparts. This finding is essential as it implies that the journey towards recovery is not solely reliant on medical treatments but can also be influenced significantly by lifestyle choices.
Moreover, survivors need to understand that incorporating physical activity into their daily lives can be achieved through gradual changes. Whether it’s enjoying a daily walk or participating in structured exercise programs, the goal is to foster a commitment to physical well-being that can sustain them for years to come. The data underscores a remarkable opportunity for cancer survivors to actively participate in their healing journey by prioritizing physical activity.
Exercise Guidelines for Cancer Survivors
For colon cancer survivors looking to optimize their recovery through exercise, the guidelines emphasize starting gradually and building intensity over time. The American Cancer Society recommends that survivors aim for at least 150 minutes of moderate-intensity activity weekly. This can include walking, swimming, or cycling, activities that are generally safe and effective for those recovering from treatment.
It is also important for survivors to engage in strength training exercises at least two days a week, as muscle health is paramount for overall physical functioning. Incorporating flexibility and balance exercises can further reduce the risk of falls and improve quality of life. Each exercise regimen should be tailored to match the individual’s abilities and limitations, always keeping the goal of enhancing overall health and well-being in mind.
Combating the Risk of Cancer Recurrence Through Exercise
For colon cancer survivors, the concern for cancer recurrence remains a pressing issue. Engaging in regular physical activity has been associated with lower recurrence rates. Exercise may help regulate hormones and inflammatory markers linked to cancer progression, thus serving as a preventative measure for survivors. One significant finding from recent studies indicated that those who maintained high levels of physical activity experienced lower rates of tumor recurrence compared to those who did not.
In summary, exercise is not just a recovery tool—it’s a crucial component in the fight against cancer recurrence. Engaging in a consistent and targeted physical activity regimen empowers survivors to take control of their health. Survivors should consult healthcare professionals to develop an exercise plan that aligns with their treatment history and personal goals, ensuring a path toward long-term health and wellness.
The Role of Community Support in Exercise for Cancer Survivors
Community support plays an essential role in encouraging colon cancer survivors to engage in regular physical activity. Social connections foster motivation and accountability, significantly increasing the likelihood of maintaining an exercise routine. Support groups, community fitness programs, and peer mentorship can provide survivors with the encouragement needed to embark on or sustain their fitness journeys.
Moreover, participating in group exercise settings not only combats feelings of isolation but also enhances the social aspect of recovery. Sharing experiences with fellow survivors can be therapeutic, creating a sense of belonging and understanding. Therefore, building community support systems around exercise can amplify the health benefits experienced by colon cancer survivors, contributing to a more robust recovery process.
Integrating Nutrition and Exercise for Optimal Recovery
For colon cancer survivors, integrating nutrition with physical activity can significantly enhance recovery outcomes. A balanced diet rich in antioxidants, fiber, and essential nutrients coupled with regular exercise can optimize health benefits. Diet plays a critical role in fueling physical activity, aiding in muscle recovery, and maintaining energy levels, thus supporting the efforts to combat cancer-related fatigue.
Furthermore, many survivors find that coupling exercise with proper nutrition helps establish effective lifestyle habits. Meal planning and preparation can become part of the exercise routine, making healthy choices more accessible. By focusing on a holistic approach that combines diet and exercise, colon cancer survivors can maximize their chances of thriving during recovery.
Recommendations for Sustaining an Active Lifestyle Post-Treatment
Sustaining an active lifestyle post-treatment can be challenging for colon cancer survivors, yet it is vital for long-term health. To maintain consistency, individuals should establish realistic goals and schedules that accommodate their recovery process. Starting with short, achievable exercise goals, such as 10-15 minute walks, can pave the way for more extensive fitness routines as strength and stamina improve.
Moreover, tracking progress through journals or fitness wearables can motivate survivors to stay active. Finding enjoyable physical activities, whether dancing, gardening, or joining local sports leagues, makes it easier to integrate exercise into daily life. Ultimately, fostering a supportive network of friends, family, or fitness communities can help survivors sustain their active lifestyles and continue reaping the health benefits of exercise.
Frequently Asked Questions
What are the exercise benefits for colon cancer survivors regarding long-term survival?
Exercise benefits for colon cancer survivors include significantly improved long-term survival rates. Research indicates that regular physical activity post-treatment can help close the survival gap between colon cancer patients and the general population, enhancing the overall health benefits of exercise and contributing to better outcomes after colon cancer treatment.
How does physical activity impact recovery for colon cancer survivors?
Physical activity plays a crucial role in exercise and cancer recovery for colon cancer survivors. Engaging in regular exercise can improve both physical and mental health, reduce fatigue, and enhance quality of life, contributing to a smoother recovery process after colon cancer treatment.
Why is physical activity essential for colon cancer survivors post-treatment?
Physical activity is essential for colon cancer survivors post-treatment because it reduces the risk of cancer recurrence, enhances long-term survival, and improves overall wellness. Studies show that survivors who participate in higher levels of exercise experience survival rates that are closer to the general population, emphasizing the health benefits of exercise in managing cancer recovery.
Can exercise help reduce disparities in survival rates for colon cancer survivors?
Yes, exercise can help reduce disparities in survival rates for colon cancer survivors. Research has demonstrated that those who maintain high levels of physical activity after treatment exhibit survival rates that are significantly better, thus narrowing the gap between colon cancer patients and their peers in the general population.
What type of exercise is recommended for colon cancer survivors for maximum benefit?
For colon cancer survivors aiming for maximum benefit, a mix of aerobic exercises such as walking, cycling, or swimming, along with strength training, is recommended. Engaging in at least 18 MET-hours of activity per week can lead to improved survival rates, underscoring the importance of sustained physical activity post-cancer treatment.
How does exercise affect the overall health of colon cancer survivors?
Exercise positively affects the overall health of colon cancer survivors by improving cardiovascular fitness, reducing fatigue, and enhancing mental health. The health benefits of exercise go beyond physical well-being, as they can also boost immunity and reduce the risk of other chronic diseases, making it a vital component of post-treatment life.
What survival rate improvements have been observed with exercise in colon cancer survivors?
Survival rate improvements observed with exercise in colon cancer survivors are significant. Those engaging in regular physical activity have experienced overall survival rates much closer to those of the general population, with studies showing up to 50.5 percent lower mortality risks in highly active patients compared to their less active counterparts.
Is any level of exercise beneficial for colon cancer survivors?
Yes, any level of exercise is beneficial for colon cancer survivors. As stated by research, even small amounts of activity can yield positive effects on health and survival. Starting with brief sessions, like taking short walks, can lead to greater engagement in physical activity and help improve outcomes after colon cancer treatment.
| Key Points |
|---|
| Exercise improves longevity for colon cancer survivors, reducing the gap in survival rates compared to the general population. |
| Physical activity post-treatment correlates with improved survival rates for stage 3 colon cancer patients. |
| Patients with low activity levels had survival rates significantly lower compared to those who maintained higher activity levels. |
| Survival rates show disparities based on physical activity; more active patients fare better overall during follow-up. |
| Both young and old patients benefit from increased physical activity, reinforcing the message that any exercise is beneficial. |
| Exercise reduces survival disparities, even for patients whose cancer recurs. |
Summary
Exercise benefits for colon cancer survivors are significant, offering a path to improved longevity and quality of life. Engaging in regular physical activity not only diminishes the survival gap between colon cancer survivors and the general population but also promotes better health outcomes post-treatment. With research from the Dana-Farber Cancer Institute showcasing the correlation between exercise levels and survival rates, it is evident that incorporating even small amounts of physical activity can lead to meaningful advancements in health. Survivors are encouraged to remain active, as this can make a crucial difference in their journey towards recovery.
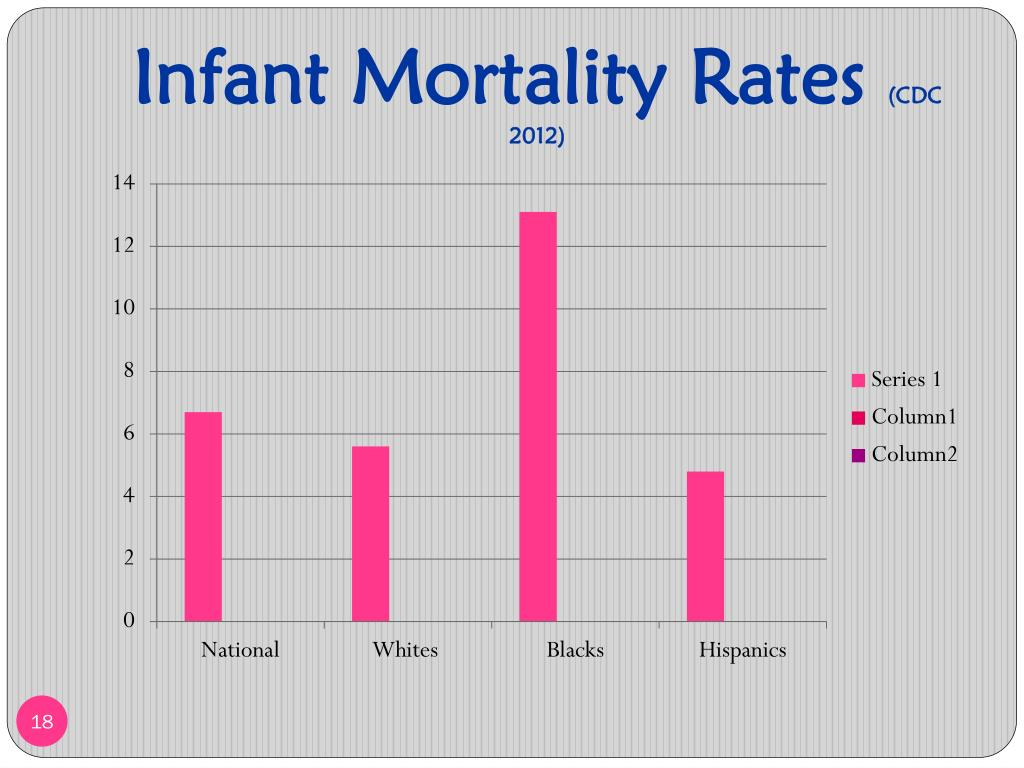
Infant Mortality Disparities: A Deepening Racial Divide
Infant mortality disparities remain one of the most pressing issues in public health, particularly when comparing Black infant deaths to those of their white counterparts. A recent study spanning 70 years reveals alarming trends: although life expectancy has improved overall, the gap between Black and white infant mortality has widened significantly. In fact, Black infants are now dying at rates that are twice as high as white infants, highlighting the severe consequences of healthcare inequality and racial health disparities. This disheartening statistic sheds light on the underlying issues surrounding healthcare access and quality, which must be addressed if we are to bridge this gap. As we delve deeper into the factors contributing to these disparities in infant mortality rates, it’s crucial to recognize the urgent need for systemic change in our healthcare system to ensure equity for all families.
When we examine the troubling trend of infant deaths, it becomes evident that the issue extends beyond mere statistics; it reflects broader societal challenges related to healthcare access and quality. Racial health inequalities have long plagued various communities, with Black infants facing disproportionately high mortality rates compared to their white peers. The findings from a comprehensive study indicate that while longevity has improved for both demographic groups, disparities in neonatal outcomes persist and have, alarmingly, grown over the decades. By understanding these life expectancy disparities through the lens of healthcare inequality, we can start to address the multifaceted nature of this crisis. As such, it is essential to initiate conversations around policy reform and healthcare practices that prioritize the well-being of all infants, regardless of their racial background.
The Widening Gap in Infant Mortality Rates
Recent research highlights a troubling trend in infant mortality rates, particularly among Black infants. Despite general improvements in life expectancy over the decades, disparities in infant deaths have widened significantly. Black infants now face a mortality rate that is 115% higher than their white counterparts, nearly doubling since the 1950s. This alarming statistic highlights not just a health crisis but a profound social injustice that cannot be overlooked.
This disparity leads to a much broader discussion about healthcare inequality in the United States. Factors contributing to this issue are multifaceted, including socioeconomic status, access to healthcare, and quality of care. Addressing these disparities requires systemic change in public health policies and a commitment to ensuring equitable healthcare for all families, regardless of race.
Understanding Racial Health Disparities
Racial health disparities remain a persistent challenge in America, with stark differences in mortality rates observable across various demographics. The broader context of healthcare inequality reveals that while there have been advancements in medical care, these improvements have not been uniformly distributed. Black Americans continue to experience higher rates of infant mortality and significantly lower life expectancies compared to white Americans.
To combat these disparities, it is critical to examine the social determinants of health that disproportionately affect Black communities. Factors such as poverty, limited access to quality healthcare, and inadequate prenatal care contribute to higher rates of infant mortality. By recognizing the underlying causes of these health inequities, policymakers can begin to implement targeted interventions aimed at reducing the mortality gap.
The Role of Public Policy in Healthcare
Public policy plays a vital role in shaping healthcare outcomes across the population. The disparities in infant mortality rates highlight an urgent need for healthcare reforms that address the systemic inequalities faced by Black Americans. Current evidence suggests that if public health officials prioritized equity in healthcare access and quality, millions of lives could be saved each year.
Effective public policies must prioritize not only the reduction of infant mortality but also overall healthcare inequality. Enhancing prenatal and maternal care services for at-risk populations, alongside investing in community-based healthcare initiatives, is crucial. This approach would not only address immediate healthcare needs but also contribute to long-term changes in health outcomes for Black infants and their families.
Examining Healthcare Access and Quality
Access to healthcare services is a fundamental determinant of health, impacting both the availability and quality of care received by individuals. For Black infants, barriers to accessing comprehensive healthcare can lead to critical delays in treatment and increased risk factors associated with higher mortality rates. The disparity in healthcare access is a reflection of the broader issues of racial injustice and inequality.
To improve healthcare access, policymakers must address both geographic and socioeconomic barriers that hinder Black families from receiving necessary prenatal and postnatal care. Initiatives that expand health insurance coverage, provide transportation assistance to medical facilities, and improve healthcare infrastructure within underserved communities can significantly enhance access to quality care and, in turn, improve infant mortality rates.
The Impact of Socioeconomic Factors
Socioeconomic status is intricately linked to health outcomes, influencing factors such as nutrition, education, and access to healthcare resources. In the case of Black infants, families with lower socioeconomic status often experience compounded stressors that negatively impact health, including limited healthcare access and poor living conditions. Addressing these socioeconomic disparities is crucial for reducing infant mortality rates.
Interventions must focus not only on direct healthcare services but also on holistic approaches that address the broader determinants of health. Programs aimed at reducing poverty through education, job training, and housing support can lead to improved health outcomes over time. By understanding and addressing these interconnected factors, it is possible to create a supportive environment that fosters healthier communities and reduces infant mortality.
Discovering Solutions to Prevent Infant Deaths
The need for actionable solutions to prevent infant deaths among Black communities is more pressing than ever. While the research indicates substantial disparities, it also calls for urgent action from public health officials and policymakers. Identifying what steps can be taken to ensure Black infants receive the care they need is critical to reversing these trends.
Solutions may involve increasing funding for maternal health programs, enhancing public health campaigns aimed at educating expectant mothers, and addressing systemic biases within healthcare institutions. Additionally, grassroots efforts that engage communities in health education and advocacy can empower families to seek out and demand equitable healthcare services, ultimately leading to improved outcomes for infants.
The Need for Continuous Research
Understanding the complexities of racial health disparities requires ongoing research and data collection. By continually studying infant mortality rates and their contributing factors, researchers can provide insights that inform policymakers and healthcare providers. Longitudinal studies, such as the recent 70-year analysis, offer essential data needed to identify trends and the effectiveness of interventions over time.
Further research should also prioritize the voices of affected communities. Engaging with families who’ve experienced infant loss can provide valuable perspectives and help shape future research directions. This community-driven approach can lead to better identification of barriers in healthcare access and inform the development of culturally competent healthcare programs aimed at reducing disparities.
Conclusion: Bridging the Gap in Healthcare Inequity
In conclusion, while improvements in life expectancy among Americans are encouraging, the increasing disparities in infant mortality rates cannot be ignored. The stark reality that Black infants are dying at twice the rate of white infants calls for a concerted effort to bridge this gap. Public policy, healthcare access, and socioeconomic factors must all be addressed to foster equity in health outcomes.
The commitment to improving healthcare equity is not just a moral imperative; it is essential for the health of the nation. By working collaboratively across sectors—government, healthcare, education, and communities—efforts can be made to ensure that all infants, regardless of race or background, have the opportunity to thrive. Only through collective action and sustained commitment can we hope to eliminate these disparities in the future.
Frequently Asked Questions
What are the main causes of infant mortality disparities between Black and white infants?
Infant mortality disparities between Black and white infants are largely attributed to healthcare inequality, specifically access to quality healthcare. Medical conditions during pregnancy significantly contribute to the higher mortality rates experienced by Black infants, emphasizing the pressing need for improved healthcare access and quality.
How have infant mortality rates changed over the last 70 years for Black infants compared to white infants?
Over the past 70 years, while overall mortality rates have improved, infant mortality rates for Black infants have become increasingly disproportionately high, with Black infants dying at almost twice the rate of white infants today. This represents a worrying trend in racial health disparities in infant mortality.
Why is there a growing concern about the widening gap in infant mortality rates since the 1950s?
The widening gap in infant mortality rates since the 1950s is concerning because it highlights persistent racial health disparities and systemic healthcare inequality. Despite improvements in life expectancy for both racial groups, Black infants continue to face disproportionately higher mortality rates, indicating a failure to adequately address these disparities.
What implications do the findings on Black infant deaths have for public health policy?
The findings on Black infant deaths underscore the urgent need for public health policy reforms aimed at reducing healthcare inequalities. Policymakers must prioritize initiatives that address the root causes of these disparities, ensuring that Black infants receive equitable healthcare access and quality comparable to their white counterparts.
How do the life expectancy disparities affect overall mortality rates among Black and white Americans?
While life expectancy has improved for both Black and white Americans, the overall mortality rates show that Black Americans have an 18 percent higher mortality rate, with infant mortality disparities remaining a critical issue. Such disparities indicate that improvements in life expectancy do not translate into equitable health outcomes for all racial groups.
What can be done to address the excess infant deaths among Black Americans?
To address the excess infant deaths among Black Americans, a multi-faceted approach is necessary, focusing on improving access to comprehensive prenatal care, enhancing the quality of healthcare services, and addressing underlying socioeconomic factors that contribute to healthcare inequality.
Are there any studies showing trends in healthcare for Black and white Americans?
Yes, studies show that while healthcare access and metrics have improved for both Black and white Americans over the past few decades, the comparison reveals persistent racial disparities. Shorter spans of research may overlook the worsening trends in specific areas such as infant mortality among Black infants.
What are the long-term effects of healthcare inequality on infant mortality rates?
Long-term healthcare inequality significantly impacts infant mortality rates, perpetuating a cycle of disparities wherein marginalized communities, particularly Black infants, continue to experience higher mortality rates. Addressing these inequalities is essential to reverse these troubling trends.
How do systemic issues contribute to racial health disparities in infant mortality?
Systemic issues such as socioeconomic factors, access to healthcare, and quality of care contribute significantly to racial health disparities in infant mortality. These underlying conditions create barriers that disproportionately affect Black infants, leading to higher mortality rates.
What role does public policy play in reducing infant mortality disparities?
Public policy plays a crucial role in reducing infant mortality disparities by strategizing effective healthcare interventions, allocating resources for equitable healthcare access, and implementing programs that address the social determinants of health affecting marginalized populations.
| Key Points | |
|---|---|
| Overall life expectancy has improved for both racial groups | Life expectancy for Black Americans increased from 60.5 to 76 years (20.4% increase), and for white Americans from 69 to 79.3 years (13% increase) |
| Mortality rates among Black and white infants | Black infants are dying at twice the rate of white infants today, with a mortality rate that is 115% higher than in the 1950s, which was 92% higher. |
| Factors contributing to infant mortality disparities | Medical conditions during pregnancy are a leading cause of excess deaths among Black infants, highlighting healthcare inequalities in access and quality. |
| Need for public policy action | Despite improvements in overall healthcare, significant gaps persist; policymakers must prioritize addressing these disparities to improve outcomes. |
Summary
Infant mortality disparities remain a serious public health issue, highlighting the urgent need for targeted interventions. While Americans are living longer, the gap in mortality rates between Black and white infants has actually widened in the past 70 years, with Black infants facing a mortality rate twice that of their white counterparts. This alarming trend points to the crucial role of healthcare access and quality in addressing these disparities. It is imperative for researchers and public health officials to focus on the underlying causes and to implement effective policy measures that ensure equitable healthcare for all infants, irrespective of race.