Exercise Benefits for Colon Cancer Survivors: Live Longer
Exercise benefits for colon cancer survivors are profound, as recent studies reveal that regular physical activity significantly enhances long-term survival rates for patients who have undergone colon cancer treatment. Engaging in consistent workouts not only aids in recovery but also helps narrow the survival gap between these survivors and the general population. Research conducted by Dana-Farber Cancer Institute indicates that patients with stage 3 colon cancer who embrace an active lifestyle experience improved survival rates compared to their less active counterparts. With colon cancer being a prevalent cause of cancer-related mortality, understanding the health benefits of exercise becomes crucial for those striving to enhance their quality of life post-diagnosis. Therefore, incorporating physical activity and cancer recovery strategies into daily routines is essential for maximizing outcomes and fostering longevity for colon cancer survivors.
The advantages of physical exercise for individuals recovering from colorectal cancer are not only scientifically substantiated but also essential for improving overall well-being. Post-cancer treatment, engaging in various forms of physical activity helps to bolster resilience and can significantly impact long-term outcomes, effectively bridging the gap in survival rates. This correlation between exercise and cancer recovery underscores the necessity for survivors to commit to an active lifestyle for better health outcomes. Studies show that maintaining a consistent regimen of physical exertion can lead to a decrease in the risks associated with cancer recurrence, while also contributing to a healthier life post-treatment. Thus, embracing physical activity emerges as a key aspect for those navigating the journey of survival after a diagnosis of colon cancer.
Understanding Colon Cancer Treatment and Recovery
Colon cancer treatment often involves a combination of surgery, chemotherapy, and ongoing monitoring. For survivors, recovery does not solely hinge on medical interventions; lifestyle factors such as nutrition and exercise play a pivotal role. Post-treatment recovery can be an arduous journey, but physical activity positively influences both mental and physical health. Engaging in regular exercise can help mitigate treatment side effects, such as fatigue and depression, thus facilitating a smoother transition back to daily life.
Research continues to shed light on the profound benefits of physical activity during recovery from colon cancer. Beyond physical improvements, exercise fosters a sense of agency among survivors, enabling them to reclaim control over their health. Simple activities, from walking to more structured exercise programs, empower individuals, contributing to overall well-being and vitality post-cancer treatment.
The Importance of Exercise for Colon Cancer Survivors
Exercise has been shown to deliver numerous health benefits for colon cancer survivors, significantly impacting their overall quality of life. A study from the Dana-Farber Cancer Institute revealed that regular physical activity can improve long-term survival rates for stage 3 colon cancer patients, narrowing the survival gap between these individuals and the general population. With physical activity linked to reduced risks of cancer recurrence, the importance of maintaining a regular exercise routine cannot be overstated.
Additionally, survivors who engage in regular exercise display improved psychological well-being. The mental health benefits of physical activity include reduced anxiety and depression levels, providing a holistic approach to recovery that encompasses both body and mind. Encouraging cancer survivors to incorporate exercise into their daily routines can lead to a substantial enhancement in their life satisfaction and emotional stability.
The Connection Between Physical Activity and Cancer Recovery
Evidence supporting the connection between physical activity and cancer recovery continues to grow. Studies highlight how survivors of colon cancer who participate in a consistent exercise regimen experience improved health outcomes compared to those who lead sedentary lifestyles. One significant finding suggests that survivors engaging in higher levels of physical activity demonstrate survival rates similar to the general population, emphasizing the role exercise plays in recovery.
Moreover, physical activity during recovery can be integral to combating treatment side effects. Weight gain, loss of muscle mass, and fatigue are common post-treatment challenges faced by survivors. Incorporating moderate-intensity activities into their daily lives helps mitigate these effects, enhancing physical fitness and health resilience. Ultimately, exercise serves as a powerful ally in the recovery journey for colon cancer survivors.
Health Benefits of Exercise for Cancer Patients
The health benefits of exercise extend far beyond physical improvements, especially for cancer patients. Regular activity can bolster the immune system, enhance cardiovascular health, and help maintain a healthy weight—critical factors for colon cancer survivors. By engaging in moderate exercise, these individuals can significantly reduce the risk of developing comorbid conditions associated with poor health outcomes post-treatment.
Additionally, exercise can serve as a psychological boost, helping cancer survivors combat feelings of isolation and stress often experienced during recovery. Group exercises or community classes can provide social support alongside physical benefits, creating a multifaceted approach to health enhancement. Research illustrates that patients who prioritize exercise not only improve their physical condition but also cultivate resilience and optimism during a challenging recovery phase.
Addressing Long-Term Survival in Colon Cancer Patients
Long-term survival after colon cancer treatment is a common concern for many patients. Engaging in regular exercise has been linked to improved long-term survival outcomes, with studies indicating that survivors who maintain an active lifestyle have much better prospects than their less active counterparts. This finding is essential as it implies that the journey towards recovery is not solely reliant on medical treatments but can also be influenced significantly by lifestyle choices.
Moreover, survivors need to understand that incorporating physical activity into their daily lives can be achieved through gradual changes. Whether it’s enjoying a daily walk or participating in structured exercise programs, the goal is to foster a commitment to physical well-being that can sustain them for years to come. The data underscores a remarkable opportunity for cancer survivors to actively participate in their healing journey by prioritizing physical activity.
Exercise Guidelines for Cancer Survivors
For colon cancer survivors looking to optimize their recovery through exercise, the guidelines emphasize starting gradually and building intensity over time. The American Cancer Society recommends that survivors aim for at least 150 minutes of moderate-intensity activity weekly. This can include walking, swimming, or cycling, activities that are generally safe and effective for those recovering from treatment.
It is also important for survivors to engage in strength training exercises at least two days a week, as muscle health is paramount for overall physical functioning. Incorporating flexibility and balance exercises can further reduce the risk of falls and improve quality of life. Each exercise regimen should be tailored to match the individual’s abilities and limitations, always keeping the goal of enhancing overall health and well-being in mind.
Combating the Risk of Cancer Recurrence Through Exercise
For colon cancer survivors, the concern for cancer recurrence remains a pressing issue. Engaging in regular physical activity has been associated with lower recurrence rates. Exercise may help regulate hormones and inflammatory markers linked to cancer progression, thus serving as a preventative measure for survivors. One significant finding from recent studies indicated that those who maintained high levels of physical activity experienced lower rates of tumor recurrence compared to those who did not.
In summary, exercise is not just a recovery tool—it’s a crucial component in the fight against cancer recurrence. Engaging in a consistent and targeted physical activity regimen empowers survivors to take control of their health. Survivors should consult healthcare professionals to develop an exercise plan that aligns with their treatment history and personal goals, ensuring a path toward long-term health and wellness.
The Role of Community Support in Exercise for Cancer Survivors
Community support plays an essential role in encouraging colon cancer survivors to engage in regular physical activity. Social connections foster motivation and accountability, significantly increasing the likelihood of maintaining an exercise routine. Support groups, community fitness programs, and peer mentorship can provide survivors with the encouragement needed to embark on or sustain their fitness journeys.
Moreover, participating in group exercise settings not only combats feelings of isolation but also enhances the social aspect of recovery. Sharing experiences with fellow survivors can be therapeutic, creating a sense of belonging and understanding. Therefore, building community support systems around exercise can amplify the health benefits experienced by colon cancer survivors, contributing to a more robust recovery process.
Integrating Nutrition and Exercise for Optimal Recovery
For colon cancer survivors, integrating nutrition with physical activity can significantly enhance recovery outcomes. A balanced diet rich in antioxidants, fiber, and essential nutrients coupled with regular exercise can optimize health benefits. Diet plays a critical role in fueling physical activity, aiding in muscle recovery, and maintaining energy levels, thus supporting the efforts to combat cancer-related fatigue.
Furthermore, many survivors find that coupling exercise with proper nutrition helps establish effective lifestyle habits. Meal planning and preparation can become part of the exercise routine, making healthy choices more accessible. By focusing on a holistic approach that combines diet and exercise, colon cancer survivors can maximize their chances of thriving during recovery.
Recommendations for Sustaining an Active Lifestyle Post-Treatment
Sustaining an active lifestyle post-treatment can be challenging for colon cancer survivors, yet it is vital for long-term health. To maintain consistency, individuals should establish realistic goals and schedules that accommodate their recovery process. Starting with short, achievable exercise goals, such as 10-15 minute walks, can pave the way for more extensive fitness routines as strength and stamina improve.
Moreover, tracking progress through journals or fitness wearables can motivate survivors to stay active. Finding enjoyable physical activities, whether dancing, gardening, or joining local sports leagues, makes it easier to integrate exercise into daily life. Ultimately, fostering a supportive network of friends, family, or fitness communities can help survivors sustain their active lifestyles and continue reaping the health benefits of exercise.
Frequently Asked Questions
What are the exercise benefits for colon cancer survivors regarding long-term survival?
Exercise benefits for colon cancer survivors include significantly improved long-term survival rates. Research indicates that regular physical activity post-treatment can help close the survival gap between colon cancer patients and the general population, enhancing the overall health benefits of exercise and contributing to better outcomes after colon cancer treatment.
How does physical activity impact recovery for colon cancer survivors?
Physical activity plays a crucial role in exercise and cancer recovery for colon cancer survivors. Engaging in regular exercise can improve both physical and mental health, reduce fatigue, and enhance quality of life, contributing to a smoother recovery process after colon cancer treatment.
Why is physical activity essential for colon cancer survivors post-treatment?
Physical activity is essential for colon cancer survivors post-treatment because it reduces the risk of cancer recurrence, enhances long-term survival, and improves overall wellness. Studies show that survivors who participate in higher levels of exercise experience survival rates that are closer to the general population, emphasizing the health benefits of exercise in managing cancer recovery.
Can exercise help reduce disparities in survival rates for colon cancer survivors?
Yes, exercise can help reduce disparities in survival rates for colon cancer survivors. Research has demonstrated that those who maintain high levels of physical activity after treatment exhibit survival rates that are significantly better, thus narrowing the gap between colon cancer patients and their peers in the general population.
What type of exercise is recommended for colon cancer survivors for maximum benefit?
For colon cancer survivors aiming for maximum benefit, a mix of aerobic exercises such as walking, cycling, or swimming, along with strength training, is recommended. Engaging in at least 18 MET-hours of activity per week can lead to improved survival rates, underscoring the importance of sustained physical activity post-cancer treatment.
How does exercise affect the overall health of colon cancer survivors?
Exercise positively affects the overall health of colon cancer survivors by improving cardiovascular fitness, reducing fatigue, and enhancing mental health. The health benefits of exercise go beyond physical well-being, as they can also boost immunity and reduce the risk of other chronic diseases, making it a vital component of post-treatment life.
What survival rate improvements have been observed with exercise in colon cancer survivors?
Survival rate improvements observed with exercise in colon cancer survivors are significant. Those engaging in regular physical activity have experienced overall survival rates much closer to those of the general population, with studies showing up to 50.5 percent lower mortality risks in highly active patients compared to their less active counterparts.
Is any level of exercise beneficial for colon cancer survivors?
Yes, any level of exercise is beneficial for colon cancer survivors. As stated by research, even small amounts of activity can yield positive effects on health and survival. Starting with brief sessions, like taking short walks, can lead to greater engagement in physical activity and help improve outcomes after colon cancer treatment.
| Key Points |
|---|
| Exercise improves longevity for colon cancer survivors, reducing the gap in survival rates compared to the general population. |
| Physical activity post-treatment correlates with improved survival rates for stage 3 colon cancer patients. |
| Patients with low activity levels had survival rates significantly lower compared to those who maintained higher activity levels. |
| Survival rates show disparities based on physical activity; more active patients fare better overall during follow-up. |
| Both young and old patients benefit from increased physical activity, reinforcing the message that any exercise is beneficial. |
| Exercise reduces survival disparities, even for patients whose cancer recurs. |
Summary
Exercise benefits for colon cancer survivors are significant, offering a path to improved longevity and quality of life. Engaging in regular physical activity not only diminishes the survival gap between colon cancer survivors and the general population but also promotes better health outcomes post-treatment. With research from the Dana-Farber Cancer Institute showcasing the correlation between exercise levels and survival rates, it is evident that incorporating even small amounts of physical activity can lead to meaningful advancements in health. Survivors are encouraged to remain active, as this can make a crucial difference in their journey towards recovery.
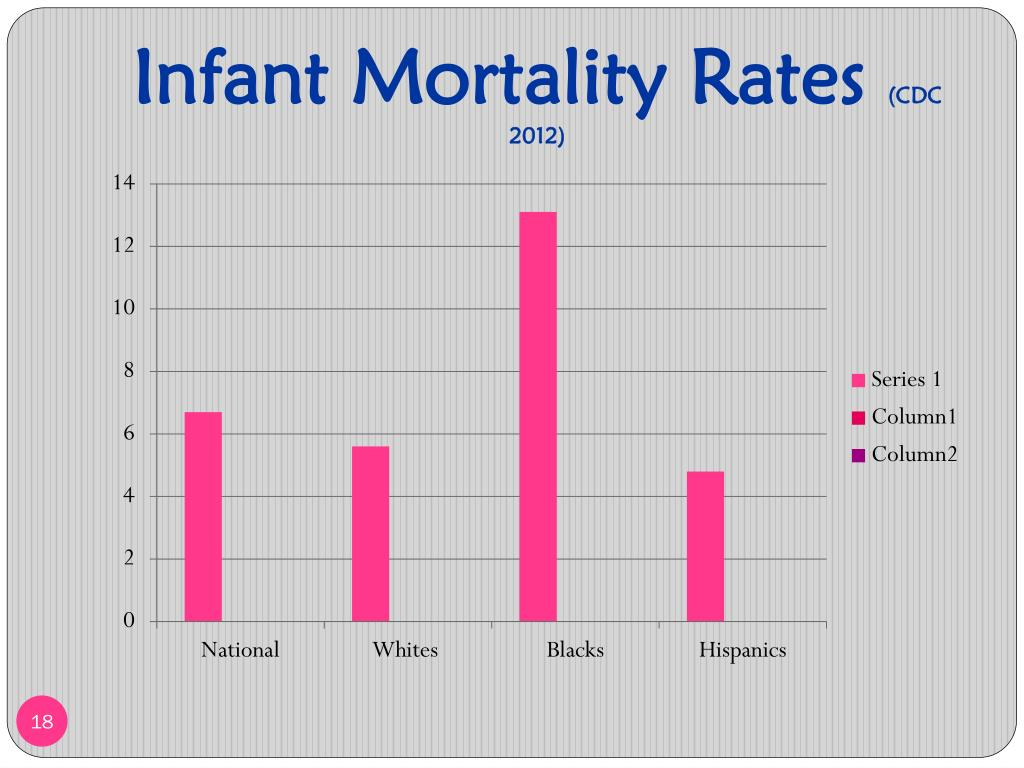
Infant Mortality Disparities: A Deepening Racial Divide
Infant mortality disparities remain one of the most pressing issues in public health, particularly when comparing Black infant deaths to those of their white counterparts. A recent study spanning 70 years reveals alarming trends: although life expectancy has improved overall, the gap between Black and white infant mortality has widened significantly. In fact, Black infants are now dying at rates that are twice as high as white infants, highlighting the severe consequences of healthcare inequality and racial health disparities. This disheartening statistic sheds light on the underlying issues surrounding healthcare access and quality, which must be addressed if we are to bridge this gap. As we delve deeper into the factors contributing to these disparities in infant mortality rates, it’s crucial to recognize the urgent need for systemic change in our healthcare system to ensure equity for all families.
When we examine the troubling trend of infant deaths, it becomes evident that the issue extends beyond mere statistics; it reflects broader societal challenges related to healthcare access and quality. Racial health inequalities have long plagued various communities, with Black infants facing disproportionately high mortality rates compared to their white peers. The findings from a comprehensive study indicate that while longevity has improved for both demographic groups, disparities in neonatal outcomes persist and have, alarmingly, grown over the decades. By understanding these life expectancy disparities through the lens of healthcare inequality, we can start to address the multifaceted nature of this crisis. As such, it is essential to initiate conversations around policy reform and healthcare practices that prioritize the well-being of all infants, regardless of their racial background.
The Widening Gap in Infant Mortality Rates
Recent research highlights a troubling trend in infant mortality rates, particularly among Black infants. Despite general improvements in life expectancy over the decades, disparities in infant deaths have widened significantly. Black infants now face a mortality rate that is 115% higher than their white counterparts, nearly doubling since the 1950s. This alarming statistic highlights not just a health crisis but a profound social injustice that cannot be overlooked.
This disparity leads to a much broader discussion about healthcare inequality in the United States. Factors contributing to this issue are multifaceted, including socioeconomic status, access to healthcare, and quality of care. Addressing these disparities requires systemic change in public health policies and a commitment to ensuring equitable healthcare for all families, regardless of race.
Understanding Racial Health Disparities
Racial health disparities remain a persistent challenge in America, with stark differences in mortality rates observable across various demographics. The broader context of healthcare inequality reveals that while there have been advancements in medical care, these improvements have not been uniformly distributed. Black Americans continue to experience higher rates of infant mortality and significantly lower life expectancies compared to white Americans.
To combat these disparities, it is critical to examine the social determinants of health that disproportionately affect Black communities. Factors such as poverty, limited access to quality healthcare, and inadequate prenatal care contribute to higher rates of infant mortality. By recognizing the underlying causes of these health inequities, policymakers can begin to implement targeted interventions aimed at reducing the mortality gap.
The Role of Public Policy in Healthcare
Public policy plays a vital role in shaping healthcare outcomes across the population. The disparities in infant mortality rates highlight an urgent need for healthcare reforms that address the systemic inequalities faced by Black Americans. Current evidence suggests that if public health officials prioritized equity in healthcare access and quality, millions of lives could be saved each year.
Effective public policies must prioritize not only the reduction of infant mortality but also overall healthcare inequality. Enhancing prenatal and maternal care services for at-risk populations, alongside investing in community-based healthcare initiatives, is crucial. This approach would not only address immediate healthcare needs but also contribute to long-term changes in health outcomes for Black infants and their families.
Examining Healthcare Access and Quality
Access to healthcare services is a fundamental determinant of health, impacting both the availability and quality of care received by individuals. For Black infants, barriers to accessing comprehensive healthcare can lead to critical delays in treatment and increased risk factors associated with higher mortality rates. The disparity in healthcare access is a reflection of the broader issues of racial injustice and inequality.
To improve healthcare access, policymakers must address both geographic and socioeconomic barriers that hinder Black families from receiving necessary prenatal and postnatal care. Initiatives that expand health insurance coverage, provide transportation assistance to medical facilities, and improve healthcare infrastructure within underserved communities can significantly enhance access to quality care and, in turn, improve infant mortality rates.
The Impact of Socioeconomic Factors
Socioeconomic status is intricately linked to health outcomes, influencing factors such as nutrition, education, and access to healthcare resources. In the case of Black infants, families with lower socioeconomic status often experience compounded stressors that negatively impact health, including limited healthcare access and poor living conditions. Addressing these socioeconomic disparities is crucial for reducing infant mortality rates.
Interventions must focus not only on direct healthcare services but also on holistic approaches that address the broader determinants of health. Programs aimed at reducing poverty through education, job training, and housing support can lead to improved health outcomes over time. By understanding and addressing these interconnected factors, it is possible to create a supportive environment that fosters healthier communities and reduces infant mortality.
Discovering Solutions to Prevent Infant Deaths
The need for actionable solutions to prevent infant deaths among Black communities is more pressing than ever. While the research indicates substantial disparities, it also calls for urgent action from public health officials and policymakers. Identifying what steps can be taken to ensure Black infants receive the care they need is critical to reversing these trends.
Solutions may involve increasing funding for maternal health programs, enhancing public health campaigns aimed at educating expectant mothers, and addressing systemic biases within healthcare institutions. Additionally, grassroots efforts that engage communities in health education and advocacy can empower families to seek out and demand equitable healthcare services, ultimately leading to improved outcomes for infants.
The Need for Continuous Research
Understanding the complexities of racial health disparities requires ongoing research and data collection. By continually studying infant mortality rates and their contributing factors, researchers can provide insights that inform policymakers and healthcare providers. Longitudinal studies, such as the recent 70-year analysis, offer essential data needed to identify trends and the effectiveness of interventions over time.
Further research should also prioritize the voices of affected communities. Engaging with families who’ve experienced infant loss can provide valuable perspectives and help shape future research directions. This community-driven approach can lead to better identification of barriers in healthcare access and inform the development of culturally competent healthcare programs aimed at reducing disparities.
Conclusion: Bridging the Gap in Healthcare Inequity
In conclusion, while improvements in life expectancy among Americans are encouraging, the increasing disparities in infant mortality rates cannot be ignored. The stark reality that Black infants are dying at twice the rate of white infants calls for a concerted effort to bridge this gap. Public policy, healthcare access, and socioeconomic factors must all be addressed to foster equity in health outcomes.
The commitment to improving healthcare equity is not just a moral imperative; it is essential for the health of the nation. By working collaboratively across sectors—government, healthcare, education, and communities—efforts can be made to ensure that all infants, regardless of race or background, have the opportunity to thrive. Only through collective action and sustained commitment can we hope to eliminate these disparities in the future.
Frequently Asked Questions
What are the main causes of infant mortality disparities between Black and white infants?
Infant mortality disparities between Black and white infants are largely attributed to healthcare inequality, specifically access to quality healthcare. Medical conditions during pregnancy significantly contribute to the higher mortality rates experienced by Black infants, emphasizing the pressing need for improved healthcare access and quality.
How have infant mortality rates changed over the last 70 years for Black infants compared to white infants?
Over the past 70 years, while overall mortality rates have improved, infant mortality rates for Black infants have become increasingly disproportionately high, with Black infants dying at almost twice the rate of white infants today. This represents a worrying trend in racial health disparities in infant mortality.
Why is there a growing concern about the widening gap in infant mortality rates since the 1950s?
The widening gap in infant mortality rates since the 1950s is concerning because it highlights persistent racial health disparities and systemic healthcare inequality. Despite improvements in life expectancy for both racial groups, Black infants continue to face disproportionately higher mortality rates, indicating a failure to adequately address these disparities.
What implications do the findings on Black infant deaths have for public health policy?
The findings on Black infant deaths underscore the urgent need for public health policy reforms aimed at reducing healthcare inequalities. Policymakers must prioritize initiatives that address the root causes of these disparities, ensuring that Black infants receive equitable healthcare access and quality comparable to their white counterparts.
How do the life expectancy disparities affect overall mortality rates among Black and white Americans?
While life expectancy has improved for both Black and white Americans, the overall mortality rates show that Black Americans have an 18 percent higher mortality rate, with infant mortality disparities remaining a critical issue. Such disparities indicate that improvements in life expectancy do not translate into equitable health outcomes for all racial groups.
What can be done to address the excess infant deaths among Black Americans?
To address the excess infant deaths among Black Americans, a multi-faceted approach is necessary, focusing on improving access to comprehensive prenatal care, enhancing the quality of healthcare services, and addressing underlying socioeconomic factors that contribute to healthcare inequality.
Are there any studies showing trends in healthcare for Black and white Americans?
Yes, studies show that while healthcare access and metrics have improved for both Black and white Americans over the past few decades, the comparison reveals persistent racial disparities. Shorter spans of research may overlook the worsening trends in specific areas such as infant mortality among Black infants.
What are the long-term effects of healthcare inequality on infant mortality rates?
Long-term healthcare inequality significantly impacts infant mortality rates, perpetuating a cycle of disparities wherein marginalized communities, particularly Black infants, continue to experience higher mortality rates. Addressing these inequalities is essential to reverse these troubling trends.
How do systemic issues contribute to racial health disparities in infant mortality?
Systemic issues such as socioeconomic factors, access to healthcare, and quality of care contribute significantly to racial health disparities in infant mortality. These underlying conditions create barriers that disproportionately affect Black infants, leading to higher mortality rates.
What role does public policy play in reducing infant mortality disparities?
Public policy plays a crucial role in reducing infant mortality disparities by strategizing effective healthcare interventions, allocating resources for equitable healthcare access, and implementing programs that address the social determinants of health affecting marginalized populations.
| Key Points | |
|---|---|
| Overall life expectancy has improved for both racial groups | Life expectancy for Black Americans increased from 60.5 to 76 years (20.4% increase), and for white Americans from 69 to 79.3 years (13% increase) |
| Mortality rates among Black and white infants | Black infants are dying at twice the rate of white infants today, with a mortality rate that is 115% higher than in the 1950s, which was 92% higher. |
| Factors contributing to infant mortality disparities | Medical conditions during pregnancy are a leading cause of excess deaths among Black infants, highlighting healthcare inequalities in access and quality. |
| Need for public policy action | Despite improvements in overall healthcare, significant gaps persist; policymakers must prioritize addressing these disparities to improve outcomes. |
Summary
Infant mortality disparities remain a serious public health issue, highlighting the urgent need for targeted interventions. While Americans are living longer, the gap in mortality rates between Black and white infants has actually widened in the past 70 years, with Black infants facing a mortality rate twice that of their white counterparts. This alarming trend points to the crucial role of healthcare access and quality in addressing these disparities. It is imperative for researchers and public health officials to focus on the underlying causes and to implement effective policy measures that ensure equitable healthcare for all infants, irrespective of race.