AI Tool for Pediatric Cancer Prediction: A Breakthrough Study
The advancement of an AI tool for pediatric cancer prediction marks a significant breakthrough in the realm of pediatric oncology. Specifically designed to analyze brain scans over time, this innovative technology demonstrates a markedly superior ability to predict relapse in pediatric cancer patients, particularly those battling gliomas. Traditional methods often fall short, leaving families anxious about cancer relapse prediction and the associated stress of frequent medical imaging. With the growing relevance of AI in medicine, this tool not only optimizes the use of magnetic resonance imaging (MRI) but also brings hope for more personalized treatment strategies. As research progresses, the implications of improved risk assessments for pediatric cancer could transform the landscape of patient care for children facing these challenges.
In the realm of childhood cancer, novel predictive tools are reshaping the landscape of treatment and care. A recently developed artificial intelligence solution focuses on forecasting the recurrence of malignant brain tumors in young patients, which could revolutionize treatment protocols. By leveraging advanced imaging techniques, this technology enhances our understanding of glioma progression and recurrence risks. The integration of AI into child healthcare promises to alleviate the burden on families, offering more precise monitoring of cancer relapse and optimized treatment plans. As we explore these innovations, the intersection of technology and medical care holds transformative potential for pediatric oncology.
Revolutionizing Pediatric Cancer Care with AI
The introduction of AI tools in pediatric cancer treatment represents a significant shift in how medical professionals approach patient monitoring and care. In recent years, AI has emerged as a crucial player in healthcare, especially regarding early predictions and diagnosis. One remarkable example is the innovative AI tool developed by experts at Harvard, which predicts the risk of relapse in pediatric cancer patients, particularly those diagnosed with gliomas. By utilizing advanced algorithms that analyze multiple brain scans over time, the AI not only enhances predictive accuracy but also alleviates the mental burden on families who undergo frequent imaging procedures.
Beyond simply predicting outcomes, the integration of AI in medical settings stands to transform the entire landscape of pediatric oncology. With the ability to synthesize vast amounts of data quickly, the AI tool significantly improves upon the traditional methods, which are often limited in scope and efficiency. As a result, doctors can make informed decisions, ensuring tailored treatment for each child. This is particularly important for pediatric patients, where the stakes are high and the emotional toll on families can be profound. The accurate predictions generated by AI pave the way for proactive measures, which could ultimately lead to better patient outcomes.
AI in Medicine: A Game Changer for Cancer Relapse Prediction
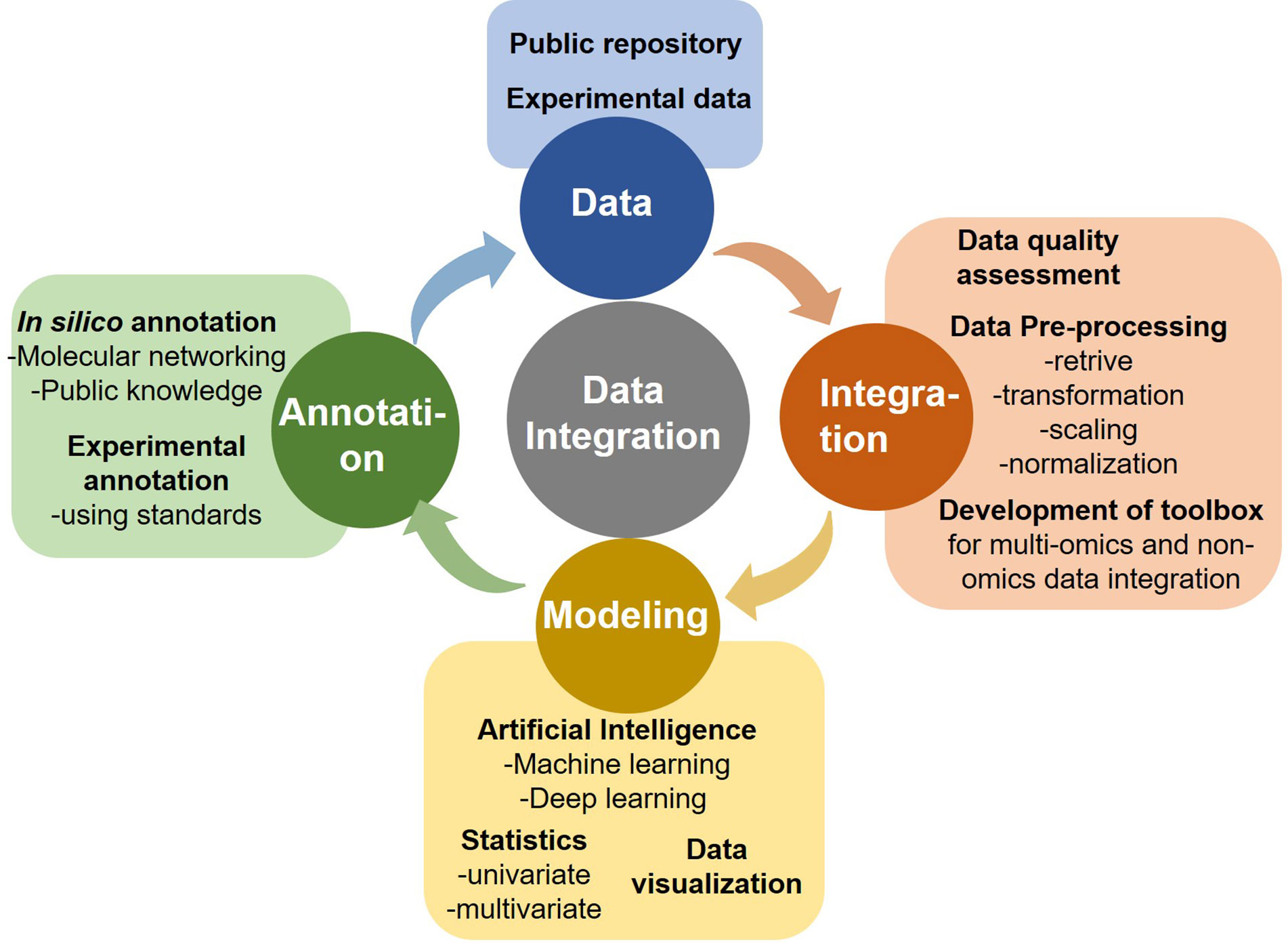
The utilization of artificial intelligence in medicine has shown immense potential, especially in the context of cancer relapse prediction. The study conducted by researchers at Mass General Brigham illustrated how AI tools can analyze serial magnetic resonance imaging (MRI) scans to forecast the likelihood of glioma recurrence. Unlike traditional practices that rely on individual scans, the AI’s temporal learning approach allows it to recognize subtle patterns and changes across multiple images over time, leading to more accurate predictions. This innovation addresses a critical need within pediatric oncology, where timely intervention could significantly impact a patient’s prognosis.
Furthermore, this groundbreaking research emphasizes the importance of harnessing technology to enhance healthcare delivery. As pediatric oncologists explore AI-powered solutions, they open doors to a new era of precision medicine. The ability to accurately predict cancer relapse empowers healthcare professionals to tailor treatment strategies, reducing the anxiety associated with frequent imaging. For families navigating the highs and lows of cancer treatment, this breakthrough provides hope and reassurance that advancements in technology can contribute to better health outcomes for their children.
Understanding Glioma Recurrence through AI Insights
Gliomas represent one of the most common types of brain tumors in children, and their unpredictable nature often leads to concern regarding potential recurrence after treatment. The research at Mass General Brigham has shed light on how AI can enhance our understanding of glioma behavior post-surgery. By employing sophisticated algorithms that analyze patterns in brain imaging over time, this AI tool has been able to predict the likelihood of glioma recurrence with impressive accuracy. Such insights are invaluable in refining follow-up protocols and treatment plans for pediatric patients.
Moreover, the implications of using AI to monitor glioma patients extend beyond just prediction. With advanced analytics, clinicians can identify which patients are most likely to benefit from additional therapies or less frequent imaging. This personalized approach not only enhances patient care but also streamlines healthcare processes, ultimately leading to more efficient use of medical resources. By understanding the dynamics of glioma recurrence through AI, healthcare providers can work collaboratively with families to ensure that each child receives optimal treatment at every stage of their journey.
The Role of Magnetic Resonance Imaging in AI Predictions
Magnetic Resonance Imaging (MRI) plays a pivotal role in monitoring pediatric patients with brain tumors, particularly gliomas. As the cornerstone of imaging in neuro-oncology, MRI provides detailed anatomical visuals that are critical for assessment and management. However, interpreting these images individually can often lead to ambiguous conclusions regarding cancer relapse. The AI tool developed by the researchers at Mass General Brigham takes this a step further by utilizing a temporal analysis of sequential MRI scans, thereby improving the precision of recurrence predictions.
The integration of MRI with AI technologies enhances diagnostic capabilities, allowing for the early identification of potential relapses in pediatric cancer patients. Utilizing data from thousands of scans, the AI model can detect minute changes in tumors that may not be immediately evident to the human eye. This capability not only supports timely intervention but also reduces the emotional stress associated with uncertain outcomes. As the field of pediatric oncology continues to embrace technological advancements, the synergy between MRI and AI represents a promising direction for improving patient management and care.
Implications of AI in Pediatric Cancer Treatment Plans
With the advent of AI tools in predicting cancer relapse, there is immense potential to reshape treatment plans for pediatric patients with gliomas. Conventional treatment strategies often follow a one-size-fits-all approach that may not account for individual patient risk factors. However, AI tools that assess MRI data over time offer a personalized framework for tailoring interventions based on precise risk assessments. This customized strategy not only reflects a deeper understanding of each child’s unique condition but also optimizes the therapeutic approach to minimize unnecessary procedures.
Moreover, as the research suggests, the AI tool could pave the way for future clinical trials aimed at validating its effectiveness in real-world settings. By categorizing patients into low-risk and high-risk groups based on AI predictions, clinicians can strategically plan follow-ups and treatments. This proactive measure could lead to a reduction in the number of imaging sessions for low-risk children, thus decreasing healthcare costs and the psychological burden on families. In essence, the implications of AI in treatment planning signify a transformative shift toward precision in pediatric cancer care.
Challenges in Implementing AI Tools in Clinical Settings
While the advantages of AI tools for predicting pediatric cancer recurrence are evident, challenges remain in their clinical implementation. One primary concern is the requirement for extensive validation to confirm that AI predictions translate effectively into everyday healthcare practices. Before such tools can be adopted on a wide scale, additional research must be conducted to address variability across different patient populations and settings. Furthermore, the establishment of protocols for integrating AI insights into clinical workflows presents its own complexities.
Healthcare professionals also face the challenge of training on new technologies, which necessitates ongoing education and adaptation within the medical community. Ensuring that staff members feel comfortable utilizing AI tools effectively is crucial for their success. Additionally, ethical considerations surrounding data privacy and the use of patient information must be carefully navigated to uphold trust within the patient community. Addressing these challenges will be vital in harnessing the full potential of AI in enhancing predictions and outcomes in pediatric cancer care.
Future Directions in Pediatric Cancer AI Research
The promising outcomes from the Harvard study indicate numerous future directions for AI research within pediatric oncology. As researchers continue to refine the algorithms for predicting glioma recurrence, exploring additional factors influencing cancer behavior could further enhance the accuracy of these tools. Future studies could investigate integrating genetic and molecular data with imaging analytics, creating a more holistic view of each patient’s cancer, and thereby improving individualized treatment strategies.
Moreover, expanding the use of AI tools beyond gliomas to other forms of pediatric cancer could amplify the impact of this technology. By applying similar predictive models, researchers may uncover valuable insights and enhance treatment protocols for various malignancies affecting children. Collaborative efforts across institutions and specialties will be crucial in advancing AI applications in oncology, reinforcing the need for partnerships among tech developers, researchers, and clinicians. As applications for AI in medicine grow, the potential to revolutionize pediatric cancer treatment appears increasingly promising.
The Importance of Collaboration in AI Research for Pediatric Cancer
Collaboration among healthcare institutions, researchers, and technology experts is essential for advancing the development of AI tools in pediatric cancer prediction. The successful research conducted by Mass General Brigham, Boston Children’s Hospital, and the Dana-Farber/Boston Children’s Cancer and Blood Disorders Center exemplifies how partnerships can lead to groundbreaking innovations. Sharing expertise, resources, and patient data allows for comprehensive studies that can produce robust findings, fostering an environment where AI can thrive in medicine.
Furthermore, these collaborative efforts pave the way for expedited validation and implementation of AI technologies. As more institutions come together to contribute to AI research, the cumulative knowledge acquired can lead to more reliable predictive models for various pediatric cancers. The collective drive toward innovation not only accelerates technological advancement but also cultivates a supportive network dedicated to enhancing the standard of care for children battling cancer. As these collaborations grow, so too does the potential for AI to reshape the landscape of pediatric oncology.
Transforming Patient Experiences with AI in Cancer Treatment
AI tools hold the promise of significantly transforming the patient experience for children undergoing treatment for brain tumors like gliomas. By improving the accuracy of relapse predictions, healthcare providers can offer families clearer insight into their child’s condition, ultimately reducing anxiety and uncertainty. With fewer unnecessary follow-up MRIs, families can focus more on the well-being of their child rather than the daunting prospect of frequent hospital visits.
Additionally, enhanced communication regarding AI findings can empower families with knowledge, allowing them to take an active role in treatment decisions. This collaborative approach fosters a sense of agency and support, creating an environment of trust between healthcare providers and families. As AI continues to evolve, its role in reshaping pediatric cancer treatment promises not only improved medical outcomes but also a more positive, less stressful experience for young patients and their families.
Frequently Asked Questions
How does the AI tool for pediatric cancer predict relapse risk?
The AI tool for pediatric cancer utilizes temporal learning to analyze multiple magnetic resonance imaging (MRI) scans over time. This technique allows it to identify subtle changes indicative of glioma recurrence, significantly improving prediction accuracy compared to traditional methods which focus on single images.
What is the significance of AI in medicine for pediatric cancer patients?
AI in medicine enhances the accuracy of cancer relapse prediction in pediatric patients, especially for brain tumors like gliomas. By leveraging insights from a series of MRI scans, the tool allows for earlier detection of potential recurrence, helping to tailor treatment and reduce stress on children and families.
How effective is the AI tool in predicting glioma recurrence?
The AI tool has demonstrated a prediction accuracy ranging from 75% to 89% for glioma recurrence one year post-treatment, compared to the approximately 50% accuracy of traditional methods that analyze isolated scans, making it a groundbreaking approach in pediatric cancer care.
What role does magnetic resonance imaging play in the AI tool for pediatric cancer?
Magnetic resonance imaging (MRI) is crucial for the AI tool, as it analyzes a sequence of scans over time. This longitudinal data helps the tool accurately predict cancer relapse, improving upon the limitations of evaluating individual MRI images.
Can the AI tool for pediatric cancer help reduce follow-up imaging?
Yes, the AI tool for pediatric cancer has the potential to reduce the need for frequent follow-up imaging. By accurately identifying low-risk patients, healthcare providers may opt for less frequent MRIs, thereby minimizing stress and burden on pediatric patients and their families.
What are gliomas and why is recurrence prediction important in pediatric cancer?
Gliomas are a type of brain tumor commonly found in children, and while many are treatable, the risk of recurrence can be high. Accurate prediction of glioma recurrence is crucial for optimizing treatment strategies and improving long-term outcomes for pediatric cancer patients.
What are the future applications of the AI tool for pediatric cancer prediction?
Future applications of the AI tool may include integrating it into clinical trials to evaluate its effectiveness in reducing unnecessary MRI scans for low-risk patients or guiding preemptive treatments for those identified as high-risk based on the AI’s predictions.
| Key Points | Details |
|---|---|
| AI Tool Overview | An AI tool that predicts relapse risk in pediatric cancer patients using brain scans. |
| Study Context | Conducted by Mass General Brigham and partners, with results published in The New England Journal of Medicine AI. |
| Temporal Learning Technique | The model uses data from multiple scans over time to improve prediction accuracy. |
| Accuracy of Predictions | The tool predicted recurrence with 75% to 89% accuracy, significantly higher than the traditional 50%. |
| Future Directions | Further validation and clinical trials needed to assess impact on patient care. |
Summary
The AI Tool for Pediatric Cancer Prediction represents a significant advancement in the ability to predict cancer relapse in pediatric patients, particularly those suffering from gliomas. This innovative tool not only enhances accuracy over traditional methods but also aims to ease the burden on families by reducing the frequency of stressful imaging follow-ups. By employing cutting-edge techniques like temporal learning, the AI can analyze changes in brain scans over time, offering hope for more personalized treatment strategies and improved outcomes for young patients.
Federal Grant Research: Key to Advancements in Health
Federal grant research plays a pivotal role in advancing public health and addressing critical issues such as nutrition and human reproduction. For researchers like Karen Emmons and Jorge Chavarro, securing funding through federal grants not only validates their efforts but also enables them to explore innovative cancer risk strategies and gather meaningful data. Emmons, who specializes in reducing cancer risk in underserved communities, highlights how obtaining a federal grant allows scientists to significantly impact the health of people by facilitating rigorous studies that adhere to the scientific review process. However, the process to obtain such grants, particularly NIH grant applications, is highly competitive and demands a substantial commitment of time and resources. As researchers strive to navigate this complex landscape, the implications of federal grant research extend beyond funding; they represent a critical lifeline to much-needed advancements in human health.
When it comes to examining governmental funding aimed at scientific exploration, the landscape of federal research grants is essential for the progress of various health disciplines. The endeavors of scholars in public health hinge on these grants, which empower them to delve into pressing issues like relationship dynamics between nutrition and reproduction and develop effective cancer mitigation tactics. Through the meticulous scientific evaluation stages, proposals undergo thorough assessments that ensure only the most promising projects receive vital financial support. The dynamic of applying for NIH funding reflects an intricate interplay of creativity, rigorous evidence, and community engagement that is foundational to impactful research. Ultimately, this systematic approach not only highlights the commitment of researchers to their fields but also brings to the forefront the critical role of resource allocation in achieving breakthroughs in health and wellness.
The Importance of Federal Grant Research in Public Health
Federal grant research is essential for public health as it provides the necessary funding for studies that address critical health issues. Researchers like Karen Emmons and Jorge Chavarro emphasize that without these grants, progress in understanding diseases and improving health outcomes would stagnate. With federal grants, researchers can undertake projects that might otherwise be impossible due to financial constraints, ultimately benefiting society at large. The significance of securing these grants cannot be overstated, as they empower researchers to seek innovative solutions to pressing health problems.
Moreover, these grants ensure that research is conducted rigorously, adhering to high standards set by funding agencies like the NIH. The rigorous application process involves detailed proposals that outline innovative approaches to existing problems. This not only promotes excellence in research but also encourages collaboration among scientists, community partners, and policymakers to tackle the complex challenges in public health. Ultimately, federal grant research plays a vital role in enhancing the lives of individuals and communities by fostering advancements in health science.
Navigating the NIH Grant Application Process
The NIH grant application process can be daunting, involving significant preparation and attention to detail. Researchers must develop a comprehensive proposal that articulates their research objectives, methodology, and anticipated outcomes. For early-career researchers like Emmons, the process starts with understanding the specific aims that align with current gaps in research, adding layers of complexity to their undertaking. Additionally, the prospect of facing a competitive landscape can be both motivating and intimidating. Gaining familiarity with the specific requirements set by the NIH is crucial, as this knowledge can significantly enhance the likelihood of a successful application.
Once a proposal is submitted, it enters a thorough scientific review process, which involves expert panels evaluating the merit and impact of the research. This review process is not only a safeguard against flawed studies but also incentivizes researchers to innovate and refine their ideas. Each section of the proposal—from the methodology to the budget—undergoes scrutiny, ensuring that every dollar requested is justified. The competitive nature of NIH funding, as defined by decreasing success rates, highlights the importance of crafting a compelling narrative that captures the essence of the research while meeting stringent scientific standards.
Building Relationships for Successful Grant Applications
A pivotal aspect of securing funding is the ability to build meaningful relationships within the research community. Emmons emphasizes the importance of collaborating with community partners who can provide insights into real-world challenges and ensure that the research aligns with public health needs. This collaborative approach not only enhances the research itself but strengthens the overall grant proposal by demonstrating to funders that the project resonates with those it aims to benefit. Networking and forming alliances with experienced researchers can provide mentorship and crucial feedback that can be invaluable during the grant application process.
Moreover, establishing these relationships can lead to more productive pilot studies, which are often necessary for demonstrating the feasibility and importance of a proposed research project. By engaging with community stakeholders and other researchers, Emmons and Chavarro can ensure that their studies address relevant issues and yield viable solutions. This alignment with community needs is increasingly favored by funding agencies as they look to support initiatives that promise tangible benefits for public health.
Maximizing Impact Through Innovative Research Designs
Successful grant applications hinge not only on robust proposals but also on innovative research designs that are responsive to evolving public health landscapes. Researchers are encouraged to think creatively when designing studies that can effectively investigate the complexities of human health. Chavarro’s work on nutrition and human reproduction exemplifies the necessity of leveraging innovative methodologies to address gaps identified in preliminary research. By utilizing cutting-edge techniques and approaches, researchers can provide insights that enhance our understanding of vital issues such as cancer prevention and reproductive health.
Additionally, incorporating multidisciplinary strategies into research designs can amplify the impact of findings and their applicability to larger populations. For instance, health-related studies that integrate perspectives from nutrition, psychology, and sociology can lead to multifaceted interventions that resonate with diverse groups. Hence, the drive for innovation in research design not only meets NIH’s standards but significantly contributes to public health advancements, ultimately supporting better health outcomes for communities.
Addressing Challenges in Funding for Public Health Research
Amidst the competitive landscape of securing federal grants, researchers frequently encounter challenges that can deter the progression of vital public health work. The recent funding freezes and administrative hurdles faced by institutions like Harvard underscore the fragility of research funding, emphasizing the importance of advocacy for continued support. Emmons’ concern regarding the sustainability of research initiatives highlights a broader issue within public health: the need for consistent and predictable funding streams to support long-term studies that can drive significant health advancements.
Moreover, the evolving regulatory landscape can complicate the research environment, forcing researchers to navigate complex compliance and reporting requirements that can distract from their primary focus of scientific inquiry. Chavarro’s insights reveal that the cuts in funding can force teams to reconsider project scopes and budgets, potentially stunting innovative research. Addressing these challenges will require collaboration among institutions, funding agencies, and the scientific community to advocate for policies that support public health research effectively.
The Role of Multidisciplinary Collaboration in Grant Success
Multidisciplinary collaboration has become increasingly essential for success in federal grant applications. Emmons and Chavarro’s research illustrates that integrating diverse perspectives and expertise enhances the quality of research proposals and can lead to more comprehensive solutions to complex health issues. Collaborating across disciplines opens new avenues for exploring innovative approaches to pressing topics, such as the intersections between nutrition, cancer risk, and reproductive health. Rather than working in isolation, researchers are better positioned to tackle multifactorial problems that require a holistic understanding.
Furthermore, fostering an environment of collaboration enriches the scientific process, making it more robust and adaptable to change. Grant proposals that showcase interdisciplinary initiatives are often favored by funding agencies, reflecting a broader recognition of the interconnected nature of health research. By leveraging the strengths of various fields, researchers can position their work as integral to advancing public health knowledge and outcomes effectively.
Feedback Mechanisms in the Grant Review Process
Receiving feedback from the scientific review groups is a crucial component of the NIH grant application process. This feedback can provide valuable insights into the strengths and weaknesses of a proposal, allowing researchers to refine their projects for future submissions. Emmons highlights that even applications that are not funded can serve as learning opportunities, enabling investigators to strengthen their proposals by addressing the reviewers’ comments. This process not only enhances the individual proposals but contributes to the overall quality of research within the field.
The iterative nature of applying for federal grants encourages researchers to continuously improve their work by leveraging knowledge gained from past experiences. Oftentimes, the feedback received can shape the direction of future research endeavors, allowing scientists to adjust their focus or methodology based on emerging trends and community needs. Therefore, the feedback mechanism in the grant review process is not just a procedural step but a vital aspect of fostering a thriving scientific community committed to progress.
Evolving Trends in Research Funding and Public Health Priorities
As public health priorities shift, so too do the trends in research funding. Current societal challenges, such as the COVID-19 pandemic, have highlighted the need for rapid responses to health crises, influencing the types of grants available. Chavarro has observed a growing emphasis on nutrition-related research within the context of comprehensive health initiatives, as funders recognize the integral role of diet in disease prevention. This evolution in focus presents both opportunities and challenges for researchers who must adapt their work to align with emerging priorities.
Additionally, as public health concerns increasingly intersect with social determinants of health, funding agencies are beginning to support research that specifically addresses issues such as health disparities and access to care. Emmons’ investigations into cancer risk among under-resourced communities illustrate the demand for research that not only delves into biological factors but also considers the broader socio-economic context. Understanding and adapting to these evolving funding trends is crucial for researchers aiming to secure support and make impactful contributions to public health.
Promoting Healthier Futures Through Innovative Research
Ultimately, the journey of securing federal grants is rooted in the researchers’ commitment to making a positive impact on public health. By investing time and effort into the grant application process, researchers like Emmons and Chavarro are not only pursuing their passion for science but are also contributing to healthier futures for communities. Their projects aim to bridge knowledge gaps and develop evidence-based strategies that empower individuals to make informed health decisions.
As researchers navigate the complexities of grant applications and funding challenges, they remain dedicated to achieving advancements that can lead to sustainable changes in public health practices. This commitment reflects the ultimate goal of scientific research: to improve quality of life and foster environments where individuals can thrive. Through their diligent work, public health researchers embody the spirit of innovation and resilience necessary to tackle the challenges of today and tomorrow.
Frequently Asked Questions
What is the importance of federal grant research in public health?
Federal grant research plays a pivotal role in public health by funding critical studies that aim to reduce health risks, such as those related to cancer and nutrition. These grants allow researchers like Karen Emmons to implement strategies that directly benefit under-resourced communities and advance health science.
How does the scientific review process affect federal grant research applications?
The scientific review process is essential for federal grant research applications, as it ensures each proposal is evaluated for its innovation, significance, and methodology. This rigorous evaluation by peer scientists helps maintain high research standards and determines which projects receive funding from entities like the NIH.
What challenges do researchers face when applying for NIH grant applications?
Researchers face various challenges when applying for NIH grant applications, including navigating a competitive review process, justifying research budgets, ensuring ethical treatment of human participants, and demonstrating that their projects fill existing gaps in knowledge, all while adhering to stringent guidelines set by the NIH.
How can researchers improve their chances of receiving funding for cancer risk strategies?
To improve their chances of receiving federal grants for cancer risk strategies, researchers should focus on building strong partnerships, staying informed on current trends, and developing innovative approaches that are well-supported by preliminary evidence. Crafting a clear and compelling application that outlines the potential impact of their research is also critical.
What are some common misconceptions about federal grant research?
A common misconception about federal grant research is that funding is readily available and easily acquired. In reality, the process is highly competitive, with low success rates for many funding programs. This emphasizes the importance of thorough preparation, robust research proposals, and understanding the requirements of the scientific review process to enhance the likelihood of grant approval.
What role does community engagement play in federal grant research?
Community engagement is vital in federal grant research as it helps researchers like Emmons connect with the populations they aim to serve. Building relationships with community partners can enhance research relevance, promote trust, and increase the likelihood that the outcomes of the research will be effectively implemented to improve public health.
How does budget justification impact NIH grant applications?
Budget justification is a critical component of NIH grant applications, as it requires researchers to clearly explain why specific expenses are necessary for their project. This includes detailing the need for equipment, materials, and staff, ensuring that funding agencies understand how each line item contributes to the overall research goals.
What is the significance of the success rates in federal grant research for public health researchers?
Success rates in federal grant research reflect the competitiveness of funding opportunities for public health researchers. For example, the National Cancer Institute had a success rate of 14.6% for R01 grants in 2023, indicating that researchers must be strategic in their proposals and often need to revise and resubmit applications after receiving feedback to secure funding.
What factors influence the evaluation of cancer research proposals by the NIH?
Factors influencing the evaluation of cancer research proposals by the NIH include the project’s innovation, significance to public health, methodological rigor, and the research team’s qualifications. Proposals are scored against one another during the scientific review process, emphasizing the need for well-rounded and compelling submissions.
Why is the NIH considered a key player in the advancement of public health research?
The NIH is considered a key player in the advancement of public health research because it provides essential financial support for cutting-edge studies that address critical health challenges. Through funding, the NIH facilitates discoveries that improve health outcomes, inform cancer risk strategies, and promote the overall well-being of populations.
| Key Point | Details |
|---|---|
| Significance of Federal Grants | Federal grants are crucial for health researchers to secure funding for studies that aim to improve public health, such as cancer risk reduction and nutrition. |
| Challenges Faced | Political changes and administrative actions, like the Trump administration’s funding freeze at Harvard, jeopardize ongoing research efforts. |
| Application Process | Writing a successful grant application involves preliminary research, building community partnerships, and navigating a rigorous review and approval process. |
| Review and Funding Rates | After application submission, proposals undergo a thorough review process with a low success rate; only about 14.6% of applications to the National Cancer Institute receive funding. |
| Impact of Funding | Secured funding allows researchers to innovate and contribute to public health significantly, yet the competition and budget constraints require careful planning. |
| Community Partnership Importance | Engaging with community partners is essential for ensuring research is relevant and impactful in under-resourced communities. |
Summary
Federal grant research is pivotal for advancing public health initiatives, evidenced by the dedicated efforts of researchers like Karen Emmons and Jorge Chavarro. Their experiences highlight not only the profound impact of this funding on scientific progress but also the inherent challenges faced by investigators. Federal grants not only empower researchers to pursue innovative solutions but also embody a partnership between academia and government that ultimately benefits society by fostering healthier communities through rigorous and evidence-based research.
Brain Cancer Prediction in Children: AI Outperforms Tradition
Brain cancer prediction in children is an emerging field that harnesses the power of artificial intelligence to revolutionize pediatric oncology. Recent studies show that AI technology significantly outperforms traditional methods in predicting glioma relapse risk, offering hope for better outcomes in young patients. This advancement could transform how we approach predicting cancer recurrence, ensuring more personalized and effective treatment plans. By utilizing innovative techniques like temporal learning in medicine, researchers are unveiling deeper insights into brain tumor dynamics over time. Consequently, improving cancer care and early intervention strategies becomes a tangible reality, enhancing survivorship in pediatric populations.
In the realm of childhood brain tumors, the prediction of cancer recurrence is gaining traction thanks to advanced machine learning techniques. The use of AI in diagnosing and monitoring pediatric tumors, particularly gliomas, represents a significant leap forward in the field of oncology. By analyzing sequential imaging data, medical professionals can now better assess the risk of tumor relapse, leading to tailored treatment regimens. As these technologies evolve, they promise to enhance the overall effectiveness of treatment and support for young patients battling these challenging conditions. Such innovations not only improve outcomes but also alleviate the burdens on families navigating the complexities of childhood cancer.
Understanding Brain Cancer Prediction in Children
The accurate prediction of brain cancer recurrence in children represents a critical challenge in pediatric oncology. Brain cancers, particularly gliomas, can exhibit varied behaviors post-surgery, making it essential for medical professionals to effectively estimate the likelihood of relapse. The development of artificial intelligence tools has proven transformative in this arena, offering enhanced predictive capabilities compared to traditional diagnostic methods. By employing sophisticated algorithms to analyze sequential MRI scans, these AI tools can track subtle changes that may indicate impending recurrence, promising to improve the experience for patients and their families.
AI is not only assisting in predicting relapse risk but is also paving the way for personalized treatment plans based on individual risk assessments. This evolving technology harnesses large datasets, such as the collection of nearly 4,000 MRI scans from pediatric patients, to train its models. As researchers refine these techniques, they hope to establish standardized protocols that integrate AI predictions into routine clinical practice, ultimately enhancing the quality of life and care for children diagnosed with brain cancer.
The Role of AI in Pediatric Oncology
Artificial intelligence is revolutionizing the landscape of pediatric oncology by providing tools that significantly outperform traditional approaches. In recent studies, AI’s ability to identify patterns in medical data has demonstrated a remarkable capacity to predict glioma relapse risk. This capability not only enhances diagnostic accuracy but also facilitates timely interventions, ensuring that high-risk patients receive the necessary attention before complications arise. Through advanced machine learning techniques, healthcare providers can now glean insights from past patient data to bolster future treatment outcomes.
Furthermore, AI-driven analysis allows for a more comprehensive understanding of each patient’s unique cancer journey. By integrating factors such as genetic predisposition and previous treatment responses, AI can inform decisions and improve cancer care strategies. The recent success of AI tools in predicting not just the presence of glioma but its potential recurrence underscores the importance of incorporating technology into oncology, yielding more targeted therapies and optimizing clinical outcomes for pediatric patients.
Temporal Learning and Its Applications in Cancer Care
Temporal learning represents a groundbreaking approach within medical imaging AI, transforming how healthcare professionals anticipate cancer recurrence. By analyzing a series of MRI scans over time rather than relying on single snapshots, this method allows AI models to capture the dynamic nature of brain tumors more accurately. The technology has revealed that subtle changes can be pivotal, providing crucial predictive insights into the likelihood of relapse for children diagnosed with gliomas.
As temporal learning techniques continue to refine the predictive abilities of AI, there is considerable hope for their application across various medical disciplines. The effective integration of these AI models into clinical settings could streamline follow-up procedures and reduce the psychological burden on families. By identifying patients at the highest risk early on, clinicians can implement preemptive strategies that could significantly impact treatment efficacy and patient well-being.
Improving Cancer Care Through AI Innovations
The evolution of AI in predicting cancer recurrence presents a substantial opportunity to improve cancer care methodologies. With innovative techniques enabling the analysis of longitudinal imaging data, healthcare providers can make informed decisions impacting patient outcomes significantly. The aim of improving care extends beyond mere prediction; it encompasses the overall experience of dealing with pediatric cancer, from diagnosis to long-term follow-up. AI innovations can lead to decreased frequency of unnecessary imaging for low-risk patients, which in turn mitigates stress for both children and their families.
Moreover, as AI tools become increasingly sophisticated, their integration into practice may support the development of tailored treatment plans. For high-risk patients, timely interventions could include targeted therapies based on specific predictive analytics derived from their imaging data. By combining technological advances with compassionate care, the overall landscape of pediatric oncology can evolve, leading to enhanced patient outcomes and experiences.
Challenges in Implementing AI in Clinical Settings
Despite the promising results observed with AI technologies in pediatric oncology, there are significant challenges to their widespread implementation in clinical settings. The necessity for further validation studies is paramount to ensure the reliability of these tools before they can be routinely integrated into care practices. Healthcare facilities must also navigate the complexities of integrating AI systems with existing medical infrastructure, ensuring that clinicians are adequately trained to utilize these new tools effectively.
Additionally, ethical considerations surrounding AI usage in patient care must be addressed. The introduction of AI in predicting cancer recurrence raises questions about data privacy, informed consent, and the potential for bias in algorithm training. Stakeholders in pediatric oncology must work collaboratively to create guidelines that secure patients’ rights while maximizing the benefits of AI technologies, fostering an environment where innovations can augment human expertise rather than replace it.
The Future of Pediatric Oncology and AI
The future of pediatric oncology is poised to be significantly influenced by advancements in artificial intelligence. As research continues to validate the efficacy of AI tools in predicting brain cancer relapse, institutions are likely to adopt these innovations more broadly. This shift may enable a radical transformation in how pediatric cancers, particularly gliomas, are monitored and treated. The integration of AI into standardized care protocols could lead to a paradigm shift, making precision medicine a reality for children facing these challenges.
Looking ahead, collaboration between technology developers, medical researchers, and clinicians will be crucial in navigating this transition. By fostering interdisciplinary partnerships, stakeholders can create robust AI systems tailored to the complexities of pediatric oncology. Continuous feedback from clinical applications will inform further refinements, ensuring that AI tools not only enhance diagnostic capabilities but also ultimately contribute to more effective, compassionate care for young patients battling cancer.
Significance of MRI in Brain Cancer Management
Magnetic resonance imaging (MRI) plays a pivotal role in the management of brain cancer in children, particularly in monitoring gliomas. The imaging technique provides detailed views of brain structures, allowing for updated assessments of tumor size and behavior. As pediatric patients undergo treatment, frequent MRI scans help clinicians detect any signs of recurrence early, which is critical for timely interventions. However, traditional methods based solely on individual scans can overlook subtle changes that might indicate a looming relapse.
With the advent of AI technologies capable of analyzing sequences of MR images, there is newfound hope for refining how these scans are used in clinical practice. By tracking transformations over time and predicting relapse with higher accuracy, AI enhances the utility of MRI. This shift not only improves diagnostic precision but also reduces the emotional burden on patients and families, enabling a more proactive approach to cancer care.
The Impact of AI on Family Experiences in Pediatric Cancer Care
The introduction of artificial intelligence tools in pediatric oncology has the potential to significantly improve family experiences during the challenging cancer journey. Traditionally, families faced extended periods of uncertainty regarding the risk of recurrence for their children diagnosed with brain tumors. With AI enhancing the accuracy of predictions regarding glioma relapse, families can receive clearer guidance regarding follow-up procedures and treatment options. This clarity helps alleviate stress and anxiety, fostering a more supportive environment for both patients and their loved ones.
Moreover, as AI aids in streamlining care processes and reducing the number of unnecessary interventions for low-risk patients, families can focus on quality time together instead of frequent medical appointments. This balance is essential for maintaining the well-being of patients and their support systems during a tumultuous time. The interplay between AI advancements and compassionate pediatric oncology will shape a more hopeful landscape for families affected by childhood brain cancer.
Collaborative Research Efforts in Pediatric Cancer Treatment
Collaborative research efforts are instrumental in advancing the use of AI technologies in pediatric oncology, particularly concerning brain cancer. By pooling resources from top institutions, clinical trials can be conducted on a larger scale, providing more comprehensive data to validate the effectiveness of AI tools. Initiatives that bring together healthcare organizations, academic institutions, and industry experts enhance knowledge-sharing and promote innovation in treatment approaches.
These partnerships are vital in pushing the boundaries of what is achievable with predictive analytics in cancer treatment. By utilizing extensive datasets, researchers can improve algorithms, ensuring they accommodate diverse patient populations. The goal is to establish AI as a reliable component of pediatric oncology that not only predicts glioma relapse but also guides personalized interventions tailored to individual patient needs, ultimately enhancing treatment outcomes and patient care.
Frequently Asked Questions
How is brain cancer prediction in children being improved by AI technologies?
AI technologies are enhancing brain cancer prediction in children by analyzing multiple brain scans over time. These AI tools utilize advanced algorithms that have significantly increased the accuracy of predicting relapse risk in pediatric glioma patients compared to traditional methods.
What role does temporal learning in medicine play in predicting brain cancer recurrence in children?
Temporal learning in medicine allows AI models to analyze sequential brain scans over time, helping to identify subtle changes that may indicate a future recurrence of brain cancer in children. This advanced technique improves the accuracy of predictions related to brain cancer recurrence.
Can AI effectively predict glioma relapse risk in young patients?
Yes, AI has proven to vastly improve the prediction of glioma relapse risk in young patients. Recent studies show that AI tools provide prediction accuracies between 75-89%, surpassing traditional single-scan methods that often only achieve about 50% accuracy.
What are the benefits of predicting cancer recurrence for children with brain tumors?
Predicting cancer recurrence using AI helps in providing targeted follow-up care and reducing the number of frequent imaging sessions that can be burdensome for children and their families. Early identification of high-risk patients could lead to timely interventions, improving overall cancer care for pediatric patients.
How do researchers gather data for AI in pediatric oncology focused on brain cancer?
Researchers collect extensive datasets, such as MR scans from pediatric patients, to train AI models. In a recent study, nearly 4,000 MR scans from 715 children were analyzed, enabling the AI tools to learn and improve their predictions regarding brain cancer recurrence effectively.
What challenges remain in implementing AI tools for brain cancer prediction in children?
Key challenges include the need for further validation of AI models across varied clinical settings and ensuring that these predictions can improve patient outcomes. Researchers aim to conduct clinical trials to test the effectiveness of AI-informed decisions in real-world scenarios.
What advances have been made in improving cancer care for children with brain tumors?
Advances such as the integration of AI tools that utilize temporal learning techniques have greatly improved the prediction of cancer recurrence. These tools help tailor follow-up care and potential treatments for children diagnosed with brain tumors, enhancing their overall treatment journey.
Why is accurately predicting brain cancer relapse critical for pediatric patients?
Accurate prediction of brain cancer relapse is critical because it aids healthcare providers in identifying children at the highest risk. This knowledge allows for more personalized and proactive treatment approaches, minimizing the harmful effects and challenges posed by recurrent brain tumors.
| Key Points |
|---|
| AI tool significantly improves brain cancer relapse prediction in children compared to traditional methods. |
| The study focused on pediatric gliomas, which can be treatable but have varying risks of recurrence. |
| Temporal learning technique allows AI to analyze multiple brain scans over time, enhancing prediction accuracy. |
| The AI model predicted recurrence of gliomas with 75-89% accuracy, a substantial improvement over traditional methods which had around 50% accuracy. |
| Further validation across different settings is necessary before clinical implementation of AI tools in pediatric care. |
| The goal is to improve care by possibly reducing unnecessary imaging or providing targeted therapies to high-risk patients. |
Summary
Brain cancer prediction in children has taken a significant leap forward with the introduction of an advanced AI tool. This tool is capable of analyzing multiple brain scans over time, which allows for better predictions of relapse risks in pediatric patients with gliomas. Traditional methods often fail to accurately determine which patients are at the highest risk of recurrence, leading to unnecessary stress and frequent imaging for families. By using a technique called temporal learning, this AI model has showcased an impressive accuracy rate of 75-89%, far exceeding previous accuracy levels. As researchers work towards the clinical application of this technology, the potential to improve patient care significantly—by minimizing imaging frequency for low-risk patients or enabling timely treatment intervention for high-risk cases—is promising. Further studies and trials will be essential in validating these findings and implementing AI tools effectively in pediatric oncology.

Cancer Research Funding: What You Need to Know
Cancer research funding plays a pivotal role in advancing our understanding and treatment of this complex disease. Securing support through federal research grants is a key milestone for public health researchers, providing them the necessary resources to explore innovative cancer risk reduction strategies. As researchers like Karen Emmons and Jorge Chavarro work tirelessly to develop life-saving interventions, they face the daunting challenge of navigating the competitive NIH grant application process. With grant success rates often hovering around 14.6%, the pressure is immense, yet the potential to make a significant impact on human health drives these dedicated scientists. The outcome of these funding endeavors not only shapes the future of cancer research but also holds the promise of transforming lives through improved healthcare solutions.
Funding for cancer research is essential for fostering groundbreaking discoveries and developing effective interventions. As scientists seek financial support through various mechanisms, including grants from federal agencies, they contribute to the broader field of public health. This funding allows researchers to implement comprehensive studies and apply sophisticated cancer risk mitigation techniques. The competitive nature of obtaining NIH grants reflects the importance of these initiatives, as only a fraction of proposals ultimately receive the coveted financial backing. Understanding the critical need for this financial support highlights the ongoing commitment to enhancing cancer prevention and treatment efforts globally.
Understanding Federal Research Grants
Federal research grants are the backbone of many scientific endeavors, providing vital funding for projects that aim to advance knowledge and improve public health. For public health researchers, such as Karen Emmons, securing these grants is not only a personal achievement but also a stepping stone towards significant contributions to society. The process can be competitive and rigorous, but it is designed to ensure that the most innovative and impactful projects receive support. Emmons recalls her first grant as a defining moment in her career, emphasizing the importance of funding in facilitating crucial research.
Moreover, the application process for federal research grants requires extensive documentation and a comprehensive understanding of both scientific principles and the funding body’s objectives. Researchers must clearly articulate their project’s goals and demonstrate how their work aligns with national health priorities. This rigorous evaluation ensures that only the most promising ideas are pursued, leading to advancements in fields such as cancer risk reduction strategies.
The Importance of NIH Grant Applications
The National Institutes of Health (NIH) plays a pivotal role in funding health-related research in the United States. For many scientists, crafting a successful NIH grant application is a challenging yet rewarding task. The process involves submitting a detailed proposal that outlines the research objectives, methodologies, and potential implications of the study. Researchers like Jorge Chavarro serve on scientific review groups, evaluating these proposals and ensuring a fair review process for all applicants.
The impact of securing an NIH grant extends beyond just financial support; it also enhances a researcher’s credibility within the scientific community. Successful applications signify a researcher’s innovative approaches and solid understanding of public health issues, which can lead to further funding opportunities and collaborations. With a success rate of only 14.6 percent for certain grants, as seen in the National Cancer Institute, persistence is key for researchers aiming to advance their work through federal funding.
Challenges Facing Cancer Research Funding
Despite the critical importance of cancer research funding, recent governmental actions pose significant threats to the continuity of support for scientific projects. The freezing of over $2.2 billion in research grants to institutions like Harvard has disrupted vital studies aimed at addressing cancer and other pressing health issues. This funding freeze creates an environment of uncertainty for researchers who rely on these funds to explore new cancer risk reduction strategies and develop life-saving treatments.
Furthermore, the ongoing political climate and government policies surrounding research funding must be navigated carefully to ensure that important work continues effectively. Researchers like Emmons highlight the necessity of public-private partnerships in driving scientific innovation and contributing to the public good. They believe that investing in research not only benefits society by improving health outcomes but also reduces overall healthcare costs, making it a vital responsibility of government.
Strategies for Successful Grant Applications
Navigating the complex landscape of grant applications is a skill that researchers develop over time. Key strategies include building strong relationships with community partners, staying informed on relevant research developments, and networking with fellow scholars. For Emmons, these strategies are critical in designing innovative studies that stand out to funding agencies. Engaging with the community ensures that the proposed research addresses real-world health challenges, making it more appealing to grant reviewers.
A well-crafted application not only highlights the significance of the research but also showcases the researcher’s qualifications and past successes. This is where a detailed biosketch comes into play, offering a comprehensive overview of the researcher’s academic history and accomplishments. By effectively communicating their research vision and the potential impact of their work, researchers can significantly improve their chances of receiving funding.
The Evaluation Process of Research Proposals
After submission, research proposals undergo a rigorous evaluation process conducted by Scientific Review Groups, which consist of volunteer scientists who assess applications based on innovation, significance, and methodology. This ensures that only the most promising and well-prepared proposals are funded. The evaluation process is designed to prioritize research that can lead to major advances in public health, including cancer research, relying heavily on the quality and originality of the proposed work.
The dual-layer review process, involving both peer evaluation and advisory council review, adds an additional layer of scrutiny that helps maintain the integrity and standards of federal funding. While the competitive nature of this process may deter some researchers, it ensures that the grants awarded align closely with national health goals and scientific priorities, ultimately benefiting public health initiatives.
Funding’s Impact on Public Health Research
Investment in public health research is crucial for developing effective interventions and strategies to combat diseases, including cancer. Federal funding not only supports researchers in their quests for breakthroughs but also fosters collaboration among institutions, government agencies, and communities. This collaborative approach is essential for translating research findings into real-world applications, particularly in under-resourced communities that face higher cancer risks.
As researchers like Emmons point out, federal research grants serve as a lifeline for projects aimed at improving health outcomes. These grants facilitate the development of evidence-based interventions that address public health disparities and promote better health practices in vulnerable populations. The connection between funding and tangible benefits to society underscores the necessity of continued investment in scientific research.
The Future of Cancer Research Funding
Looking to the future, the landscape of cancer research funding may be influenced by shifting political priorities and budgetary constraints. Researchers must stay adaptive and responsive to these changes to secure the necessary funding for their vital work. This may involve exploring alternative funding sources, such as private foundations and philanthropic organizations, alongside traditional federal research grants.
Furthermore, the innovative nature of cancer research requires a continuous dialogue between researchers, policymakers, and funding agencies. By highlighting the societal benefits of cancer research and advocating for adequate funding, researchers can help ensure that critical studies receive the support they need to advance knowledge and improve health outcomes for future generations.
Navigating Grant Resubmission Challenges
The reality of grant funding is that many applications are initially rejected. However, the process of revision and resubmission provides an invaluable opportunity for researchers to refine their proposals based on feedback from peer reviews. This iterative process not only improves the quality of their applications but also enhances the researcher’s ability to articulate their vision and the potential impact of their work more effectively.
Both Chavarro and Emmons emphasize the importance of resilience in the face of rejection. They encourage researchers to view feedback as a crucial element in developing stronger proposals for future rounds of funding. Through this process, researchers can adapt their goals and methods to better align with the priorities of funding agencies, ultimately improving their chances of success in the highly competitive environment of federal research grants.
The Role of Partnerships in Enhancing Research Outcomes
Partnerships between research institutions, community organizations, and government agencies play a vital role in advancing public health initiatives. Collaborative efforts not only strengthen research proposals but also enhance the relevance and impact of the findings. Emmons’ work in cancer risk reduction exemplifies how partnerships can lead to more effective research outcomes that directly address community health needs.
These collaborations create a feedback loop where researchers gain insights into the challenges faced by communities, enabling them to design studies that are both applicable and impactful. By recognizing the importance of partnerships, researchers can build comprehensive programs that leverage collective expertise and resources, ultimately driving innovation and improving public health. This interconnected approach underscores the value of integrative research in shaping a healthier society.
Frequently Asked Questions
What is cancer research funding and why is it important?
Cancer research funding refers to financial support provided for studies aimed at understanding, preventing, and treating cancer. It is crucial because it enables public health researchers to conduct innovative projects that can lead to groundbreaking discoveries and improved cancer risk reduction strategies. By securing federal research grants, researchers can advance scientific knowledge and develop effective treatments that ultimately save lives.
How can I apply for federal research grants for cancer research?
To apply for federal research grants related to cancer, such as those from the NIH, researchers must follow a structured application process. This typically begins with developing a strong concept that addresses a specific cancer-related issue, building partnerships, and preparing a detailed NIH grant application. It’s important to demonstrate innovation, significance, and a rigorous methodology. The process culminates in submitting the application for review by Scientific Review Groups.
What are the success rates for NIH grant applications focused on cancer research?
The success rates for NIH grant applications can vary significantly; for example, the National Cancer Institute had a success rate of approximately 14.6 percent for the common R01 grant in 2023. This indicates that while many proposals undergo extensive preparation, only about one in six applications receives funding, highlighting the competitive nature of cancer research funding.
What challenges do public health researchers face in cancer research funding?
Public health researchers often face several challenges in cancer research funding, including intense competition and the rigorous standards of NIH grant applications. Researchers need to build strong proposals backed by solid evidence, which can require significant time and collaboration with community partners. Additionally, fluctuations in government funding priorities can create uncertainty in securing necessary resources for important research initiatives.
What role do ethical considerations play in cancer research funding applications?
Ethical considerations are paramount in cancer research funding applications, especially when research involves human participants. Researchers must outline comprehensive strategies for ensuring the ethical treatment of subjects in their NIH grant applications. This includes obtaining informed consent and ensuring participants’ rights and well-being, which are carefully reviewed by oversight bodies before granting funding.
How has government funding historically impacted cancer research?
Government funding has historically played a critical role in advancing cancer research. By investing in public health initiatives, federal research grants have funded innovative projects that lead to significant improvements in cancer treatments and health outcomes. This partnership demonstrates a commitment to using cancer research funding as a means to enhance public health and reduce overall healthcare costs associated with cancer care.
| Key Points | |
|---|---|
| Research Significance & Impact | Federal grants allow researchers, like Karen Emmons, to address healthcare issues, including cancer risk. |
| Funding Challenges | The Trump administration’s $2.2 billion grant freeze has disrupted crucial research at Harvard. |
| Grant Application Process | Grant applications require extensive collaboration, innovation, and detailed project descriptions, often exceeding 100 pages. |
| Importance of Scientific Review | Applications are rigorously reviewed by Scientific Review Groups to ensure merit before funding is allocated. |
| Funding Success Rates | At the National Cancer Institute, success rates for major grants like R01 were only 14.6% in 2023. |
| Public-Private Partnership | Emmons highlights the partnership between universities and the government as essential for public health and innovation. |
Summary
Cancer research funding plays a critical role in advancing healthcare and improving lives. As demonstrated by the efforts of researchers like Karen Emmons and Jorge Chavarro, the path to obtaining funding is challenging yet rewarding, involving meticulous planning, community collaboration, and a rigorous review process. Despite recent funding freezes, the commitment to securing grants remains essential for fostering innovation in cancer research and public health.

Alzheimer’s Disease Research: Insights from Beth Stevens
Alzheimer’s disease research is at the forefront of scientific exploration, aiming to unravel the complex mechanisms behind this devastating condition. Under the leadership of pioneering neuroscientist Beth Stevens, significant advancements have been made in understanding the role of microglial cells, which act as the brain’s immune defenders. These cells are crucial for maintaining neuronal health by removing debris and refining synaptic connections, yet their malfunction can contribute to neurodegenerative diseases like Alzheimer’s. Findings from the Stevens Lab at Boston Children’s Hospital highlight how abnormal microglial activity can lead to the progression of such disorders, paving the way for innovative Alzheimer’s treatment strategies. As the aging population in the United States continues to grow, the urgency for effective therapies has never been more critical.
In the realm of neurodegenerative disease exploration, advances in Alzheimer’s disease research are crucial for understanding and combating cognitive decline. Innovators like Beth Stevens are reshaping our knowledge of the brain’s immune response through the study of microglial cells, which are vital for neural maintenance and repair. These immune cells help protect the brain by eliminating waste and optimizing neural connections, yet dysregulation in their function can exacerbate conditions like Alzheimer’s. The insight generated from studies at institutions like Boston Children’s Hospital is not only essential for early detection but also for developing impactful treatments for millions affected by these conditions. As research delves deeper into immune mechanisms and their implications for brain health, the prospects for combating Alzheimer’s continue to evolve.
Understanding the Role of Microglial Cells in Alzheimer’s Disease
Microglial cells are integral to brain health and play a crucial role in the progression of Alzheimer’s disease. These immune cells are responsible for maintaining homeostasis in the central nervous system (CNS) by continuously monitoring the brain environment. Their primary functions include clearing out dead neurons, managing inflammation, and supportively reshaping synapses. Recent studies have indicated that dysfunctional microglial activity can contribute to the pathogenesis of neurodegenerative diseases such as Alzheimer’s, where excessive synaptic pruning may lead to cognitive deficits. Thus, understanding how microglial cells operate can unveil potential therapeutic targets for Alzheimer’s treatment.
Research led by Beth Stevens at Boston Children’s Hospital has revealed that microglial cells do not merely act as passive scavengers; instead, they actively participate in the brain’s development and response to injury. By studying these cells, scientists have started to identify biomarkers that could signal the onset of Alzheimer’s disease even before symptoms manifest. This discovery is pivotal because early detection can significantly change the management of Alzheimer’s, leading to timely interventions and potentially slowing the disease’s progression. The ongoing exploration of microglial function is reshaping our understanding of neurodegenerative disease pathology.
Beth Stevens: Pioneering Research in Neurodegenerative Diseases
Beth Stevens has emerged as a leading figure in the field of neuroscience, particularly in her innovative research on microglial cells and their connection to neurodegenerative diseases. Her dedication to uncovering the complexities of the brain’s immune system has been instrumental in changing the landscape of Alzheimer’s research. Through her efforts at the Stevens Lab, she has illuminated how improper microglial pruning processes can exacerbate conditions like Alzheimer’s and Huntington’s diseases. By focusing on these immune cells, Stevens is paving the way for novel therapies that target the underlying mechanisms of neurodegeneration.
Stevens’ groundbreaking work is not only crucial for basic science but also has profound implications for public health as the incidence of Alzheimer’s continues to rise. With predictions suggesting a doubling of cases by 2050, Stevens’ research could lead to earlier diagnosis and more effective treatments, relieving the estimated financial burden associated with caregiving. This highlights the importance of continued funding and support for scientific discoveries that drive innovation in Alzheimer’s treatment and ultimately improve the quality of life for millions affected by the disease.
The Impact of Federal Funding on Alzheimer’s Research
Federal funding plays a critical role in advancing research on Alzheimer’s and other neurodegenerative diseases. For researchers like Beth Stevens, support from institutions like the National Institutes of Health (NIH) has been vital for fostering innovative ideas. These resources provide the necessary tools and platforms for scientists to investigate intricate biological systems, including the functions of microglial cells in neurodegeneration. Without this backing, many fundamental studies could remain unexplored, stalling progress in understanding diseases like Alzheimer’s.
The strategic allocation of federal funds directs focus on high-impact areas within Alzheimer’s research, facilitating developments in novel therapies and biomarkers. As the aging population continues to grow, the urgency for effective Alzheimer’s treatment escalates. This funding not only nurtures existing research but also motivates upcoming scientists to pursue careers in neuroscience, ensuring that momentum in Alzheimer’s research continues to build. Investing in research today promises significant returns in health outcomes and economic savings tomorrow.
Neuroscience Breakthroughs: A Path to Alzheimer’s Treatment
Neuroscience breakthroughs are continuously reshaping the pathways we understand Alzheimer’s disease and its treatment options. Through ongoing studies, researchers are identifying how various cellular mechanisms, particularly involving microglial cells, contribute to neurodegeneration. Beth Stevens’ research has illuminated how selective synaptic pruning can lead to loss of neuronal connections, impacting cognition. By making sense of these complex interactions, scientists can explore innovative treatment strategies that may enhance brain health and restore lost functions associated with Alzheimer’s.
Furthermore, with an emphasis on the relationship between genetic factors and neurodegenerative diseases, the field is witnessing a wave of exciting developments. The identification of new biomarkers associated with microglial function opens avenues for early detection, allowing healthcare providers to act preemptively. As this field evolves, there is potential for personalized treatment regimes that target specific pathways involved in Alzheimer’s, increasing the effectiveness of therapeutic interventions and providing hope to millions affected by cognitive decline.
Boston Children’s Hospital: Hub of Alzheimer’s Innovations
Boston Children’s Hospital has positioned itself as a leading institution in the fight against Alzheimer’s, hosting pioneering researchers such as Beth Stevens. The collaboration between the hospital and the Broad Institute of MIT and Harvard primes the environment for groundbreaking discoveries related to neurodegenerative diseases. As a center that emphasizes a multidisciplinary approach, it attracts diverse talents in neuroscience and immunology, fostering an ecosystem where innovative ideas can flourish and lead to significant advancements in Alzheimer’s treatment.
The research conducted within the walls of Boston Children’s Hospital does not just focus on symptom management but seeks to unravel the very mechanisms behind diseases like Alzheimer’s. By integrating basic science with clinical applications, researchers aim for tangible outcomes that transcend laboratory findings. As the knowledge generated here feeds into broader medical practices, it offers hope for improved diagnostic tools and more effective therapies, benefiting patients and families affected by Alzheimer’s disease.
Innovative Therapies Emerging from Alzheimer’s Research
The relentless pursuit of innovative therapies has become a hallmark of Alzheimer’s research. Thanks to pioneering scientists like Beth Stevens, new treatment avenues focused on modulating microglial cells are being explored. Understanding how these cells can be harnessed to optimize synaptic pruning opens the door for the development of drugs that may prevent or reverse cognitive decline associated with Alzheimer’s. Harnessing the immune system’s capabilities offers promising therapeutic strategies that could fundamentally alter the course of the disease.
Innovation in the pharmaceutical realm is also inspired by the fundamental neuroscience studies that elucidate the complexities of Alzheimer’s. Collaborative efforts within academic institutions and industry are yielding novel compounds aimed at enhancing microglial function, thereby improving neuronal health. As this area of research matures, we may witness a shift in the standard care model for Alzheimer’s, bringing forth treatments that target the disease at its source and enhancing the lives of those impacted.
The Future of Alzheimer’s Care: Lessons from Research
The future of Alzheimer’s care lies firmly rooted in the lessons learned from ongoing research efforts. As Beth Stevens and her colleagues delve deeper into the mechanics of microglial involvement, the insights gained are poised to reshape our understanding of disease management. A comprehensive approach that combines basic science with patient care will inform future clinical practices. This alignment ensures that treatment strategies evolve such that they are informed by the latest discoveries in neuroscience.
Moreover, improving the quality of care for Alzheimer’s patients will necessitate a paradigm shift in how we approach neurodegenerative diseases. The advancements in research underscore the importance of not only developing medications but also increasing public awareness and understanding of Alzheimer’s. Initiatives focused on education, early detection, and community support will complement medical advancements, ultimately enhancing the overall efficacy of care and preserving dignity for those navigating the complexities of Alzheimer’s.
Microglial Cells: The New Frontier in Alzheimer’s Research
Microglial cells have emerged as a new frontier in Alzheimer’s research, capturing the attention of scientists worldwide. Beth Stevens’ groundbreaking investigations into these cells reveal their pivotal role not just in maintaining brain health but also in the progression of Alzheimer’s disease. As the brain’s immune responders, microglial cells interact with neurons to ensure cerebral homeostasis, but when dysfunction arises, they may inadvertently contribute to neurodegeneration through excessive synaptic pruning. Understanding these processes is vital for designing targeted interventions that leverage microglial capabilities in therapeutic frameworks.
The potential implications of microglial cell research are profound, as they may not only lead to advancements in Alzheimer’s treatment but also offer insights relevant to other neurodegenerative diseases. By elucidating the pathways that govern microglial behavior, researchers can pave the way for innovative strategies that restore balance in the brain’s microenvironment. Thus, the pursuit of knowledge surrounding microglial cells stands at the forefront of efforts to combat Alzheimer’s disease and improve the lives of millions worldwide.
Collaboration in Alzheimer’s Research: A Necessity for Progress
Collaboration in Alzheimer’s research is paramount for driving progress, especially in the complexities surrounding neurodegenerative diseases. Institutions like Boston Children’s Hospital foster environments where multidisciplinary teams can converge to share insights and tackle the challenges posed by Alzheimer’s. Collaborative efforts between neuroscientists, clinicians, and biochemists enable the integration of diverse perspectives, which is essential for uncovering comprehensive solutions to the pressing issues of disease management and treatment.
The synergy created through such partnerships enhances the potential for breakthroughs, as researchers can pool resources and expertise to explore groundbreaking concepts in Alzheimer’s treatment. With significant progress already achieved by teams studying microglial cells under the leadership of scientists like Beth Stevens, collaboration serves as a catalyst for new discoveries that have the power to transform the landscape of Alzheimer’s care. This interconnected approach aligns science closely with patient needs, ultimately leading to better health outcomes.
Frequently Asked Questions
What is the significance of Beth Stevens’ research on microglial cells in Alzheimer’s disease research?
Beth Stevens’ research on microglial cells is pivotal in Alzheimer’s disease research as it reveals how these brain immune cells prune synapses. Aberrant pruning by microglia can lead to neurodegenerative diseases, including Alzheimer’s, by impairing synaptic health. Her findings contribute to developing new treatments and biomarkers, which are crucial for early detection of Alzheimer’s disease.
How do microglial cells contribute to the understanding of neurodegenerative diseases like Alzheimer’s?
Microglial cells play a critical role in neurodegenerative diseases such as Alzheimer’s by maintaining brain health through synaptic pruning. However, when this process goes awry, it can contribute to disease progression. Research led by Beth Stevens at Boston Children’s Hospital highlights the importance of understanding microglial function in order to develop effective therapies and intervention strategies for Alzheimer’s disease.
What role does Boston Children’s Hospital play in advancing Alzheimer’s treatment research?
Boston Children’s Hospital is at the forefront of Alzheimer’s treatment research, particularly through the work of scientists like Beth Stevens. The hospital’s partnership with the Broad Institute and its focus on microglial cells have facilitated groundbreaking discoveries that enhance understanding of Alzheimer’s disease and promote the development of new, targeted treatments for patients.
What are the implications of Stevens’ findings for Alzheimer’s disease treatment in the future?
Stevens’ findings suggest that targeting microglial function could lead to innovative treatments for Alzheimer’s disease. By understanding how microglial cells participate in synapse pruning and their overall role in brain health, researchers can develop new therapeutic strategies aimed at improving cognitive function and slowing disease progression among the millions affected by Alzheimer’s.
Why is basic science crucial for breakthroughs in Alzheimer’s disease research?
Basic science is vital for breakthroughs in Alzheimer’s disease research because it lays the foundational knowledge necessary to understand complex biological processes. Researchers like Beth Stevens emphasize that exploring fundamental mechanisms, such as microglial activity, can lead to unexpected discoveries that ultimately translate into effective treatments for Alzheimer’s and other neurodegenerative diseases.
| Key Point | Details |
|---|---|
| Research Significance | Explores the role of microglial cells in the brain’s immune response, crucial for understanding Alzheimer’s. |
| Microglial Cells Role | They clear damaged cells and prune synapses, impacting neurodegenerative diseases like Alzheimer’s. |
| Transformative Findings | Aberrant pruning of synapses potentially contributes to Alzheimer’s and similar disorders. |
| Future of Treatment | Stevens’ research lays the groundwork for new medicines and early detection biomarkers. |
| Increasing Impact | With millions affected by Alzheimer’s, Stevens’ findings could significantly impact treatment costs and management. |
Summary
Alzheimer’s disease research is at a pivotal point, driven by groundbreaking discoveries by scientists like Beth Stevens. Her exploration of microglial cells highlights how crucial these immune cells are in the context of neurodegenerative diseases, particularly Alzheimer’s. Stevens’ work suggests that improper synaptic pruning can contribute to brain deterioration, which not only helps in understanding the disease’s mechanisms but may also lead to innovative treatments. As the population ages and the prevalence of Alzheimer’s is expected to rise dramatically, research like this is critical to developing effective interventions and improving the lives of millions affected by the disease.
Youth Flourishing: Study Reveals Concerns for Future Generations
Youth flourishing is an increasingly vital topic in discussions about well-being among youth, particularly in light of recent global studies highlighting alarming trends. Researchers emphasize the necessity of investing in youth as they are the backbone of future flourishing nations—without proper support, the next generation may struggle with well-being and development. The data collected reveals that financial security alone isn’t a guarantee of successful outcomes; rather, holistic approaches are needed to encompass health, relationships, and meaning. With economic development and youth flourishing being interlinked, it is essential to understand the broader implications of youth mental health and happiness for long-term prosperity. This insight is crucial not only for policymakers but also for communities aiming to create supportive environments conducive to the holistic growth of their youth.
Investing in the younger generation’s potential is crucial for their overall happiness and development. Following the insights from a major global study, the focus extends beyond mere financial metrics to the essence of nurturing relationships and cultivating a sense of purpose among the youth. As nations strive for economic growth, understanding the nuances of youth well-being becomes paramount. This approach transcends traditional measures of success, advocating for a more comprehensive framework that includes emotional resilience, supportive communities, and spiritual fulfillment. By prioritizing these elements, societies can foster an environment where youth not only survive but truly thrive, embodying the principles of flourishing.
The Importance of Investment in Youth Well-Being
Investing in youth well-being is fundamental for the sustainable development of society. Following the findings from the Global Flourishing Study, it is evident that financial resources alone do not guarantee happiness or character development among young people. Many middle-income countries have managed to cultivate strong community ties and meaningful relationships despite having less wealth than their upper-income counterparts. This realization beckons us to rethink our strategy on how we support youth through policies that focus on emotional and social well-being rather than solely on economic metrics.
The study’s results clearly indicate that neglecting the nurturing aspects of youth development can lead to troubling outcomes. As nations grapple with rising mental health issues among young people, it’s crucial to redirect resources and attention towards fostering environments where youth can flourish. Investing in programs that enhance community engagement, mentoring opportunities, and emotional resilience can yield profound benefits, creating a generation that is not only economically productive but also socially responsible.
Youth Flourishing: A Global Perspective
Youth flourishing transcends borders and economic statuses, as highlighted by the Global Flourishing Study’s findings. Countries with vastly different economic contexts, such as Indonesia and the U.S., showcase that vibrancy and relational quality among youth are influenced by cultural values and social practices rather than mere wealth. Ensuring that youths experience meaningful relationships and find purpose in their communities is crucial, as it establishes a foundation for their overall well-being.
Moreover, the research prompts us to consider how engagement in religious and social activities contributes to youth flourishing. Across various cultures, a strong correlation exists between childhood experiences of support, whether through family ties or community involvement, and adult well-being. Exploring these dynamics not only enriches our understanding of what constitutes a life well-lived but also highlights the importance of nurturing environments that prioritize the flourishing of young individuals.
Challenges Facing Youth in Wealthy Nations
Wealthy nations face unique challenges regarding the well-being of their youth. Despite having abundant financial resources, countries like the U.S. rank lower in youth flourishing indicators compared to some developing nations. This paradox raises critical questions about the effectiveness of current societal structures in promoting holistic well-being among the younger generation. Factors such as high-pressure educational environments, loneliness, and disconnection from community can undermine the potential for prosperity, leading to feelings of discontent.
To combat this distressing trend, it is imperative for policymakers and community leaders to take proactive measures. This includes revising educational curricula to incorporate emotional and social learning, fostering a sense of belonging, and promoting mental health awareness among youth. Understanding the nuances of how economic development can impact well-being is essential to creating supportive frameworks that enable youth to thrive, not just survive.
The Role of Relationships in Youth Flourishing
Relationships play a pivotal role in the flourishing of youth. According to the Global Flourishing Study, countries where young people report having strong familial and social ties tend to show higher levels of happiness and life satisfaction. Healthy relationships contribute significantly to a sense of belonging, emotional security, and purpose. As such, initiatives that foster close familial connections and community engagement should be prioritized in youth programs to enhance their overall well-being.
Furthermore, the findings underscore the importance of mentorship and peer support networks in shaping the experiences of youth. Programs that connect young individuals with mentors not only provide guidance but also encourage youth to pursue their interests and ambitions in a supportive environment. By investing in systems that promote relationship-building, societies can help ensure that young people have the necessary support structures in place for a flourishing life.
Rethinking Economic Growth and Its Impact
The relationship between economic growth and youth flourishing is complex, as revealed by the Global Flourishing Study’s findings. While many affluent nations have built strong economies, this does not automatically translate to increased happiness or life satisfaction among their young populations. The study challenges the traditional models that equate wealth with well-being, instead advocating for a paradigm shift toward holistic approaches to human development.
Policymakers must critically assess the impacts of purely economic-focused strategies, recognizing that the emotional and social well-being of youth is paramount. Economic growth strategies should incorporate measures to enhance community engagement, social support, and access to mental health resources, thereby fostering environments conducive to flourishing. A multi-faceted approach that values relationship-building alongside financial success will be key to nurturing the next generation.
Cultural Perspectives on Youth Well-Being
Cultural contexts significantly influence the well-being of youth, as demonstrated by the diverse results of the Global Flourishing Study. Nations like Mexico and Indonesia, despite their economic challenges, showcase higher levels of youth flourishing due to their strong interconnectedness and cultural practices emphasizing community support. In contrast, while wealthier nations may present more resources, they often lack these critical cultural elements that nourish the human spirit.
Understanding the cultural nuances that contribute to youth well-being can provide valuable insights for policymakers aiming to enhance youth flourishing. By adopting best practices from various cultures that prioritize connectedness, purpose, and meaning, societies can adapt methods to support their youth in thriving. The role of culture in shaping positive youth outcomes must not only be acknowledged but actively integrated into approaches designed to bolster young people’s well-being.
The Importance of Measuring Well-Being in Youth
Measuring youth well-being is essential for understanding the multifaceted aspects of their lives, as highlighted by the Global Flourishing Study. Traditional metrics of success often focus on economic indicators, overlooking critical dimensions such as mental health, relationships, and personal fulfillment. Accurate assessments of youth well-being require holistic data that incorporates various factors affecting their lives, from family dynamics to community engagement.
To enhance youth development initiatives, it is crucial to adopt measurement tools that provide a comprehensive view of what it means to flourish. These insights not only inform interventions but also empower young people to engage in their developmental journeys more intentionally. By prioritizing holistic well-being assessments, societies can better address the unique challenges facing youth today.
Fostering Resilience Among Youth
Resilience is a crucial element in promoting youth flourishing, acting as a buffer against life’s challenges. The Global Flourishing Study emphasizes the importance of nurturing resilience through educational and community programs. By equipping young people with coping strategies and emotional intelligence, societies can foster a generation better prepared to navigate adversity and thrive despite difficulties.
Implementing resilience-building programs within schools and community centers can help cultivate supportive environments where youth feel empowered. Activities that encourage problem-solving, adaptability, and emotional regulation not only enhance individual well-being but also contribute to the overall flourishing of communities. It is essential for stakeholders to focus on these areas, ensuring youth have the tools necessary for personal and collective success.
Longitudinal Studies: Understanding Youth Development Over Time
Longitudinal studies, such as the Global Flourishing Study, provide crucial insights into the long-term developmental trends of youth. By following individuals over time, researchers can identify pivotal moments that influence well-being and flourishing. This approach allows for a deeper understanding of how early experiences shape later outcomes, making it easier to implement effective interventions tailored to specific needs.
Such studies can highlight the significance of continuous investment in youth development, revealing how early support leads to positive outcomes in adulthood. Lessons learned from longitudinal data can inform policy decisions and resource allocation, ensuring that investments are strategically directed toward enhancing the well-being of youth across all stages of their development.
Frequently Asked Questions
What is youth flourishing and why is it important for well-being among youth?
Youth flourishing refers to the holistic well-being of young people, encompassing health, happiness, meaning, and strong relationships. It is crucial for well-being among youth as it affects their overall development and future opportunities, influencing both personal satisfaction and societal progress. Investing in youth flourishing leads to better outcomes not only for individuals but also for communities and nations.
How does investment in youth contribute to flourishing nations?
Investment in youth is foundational for flourishing nations, as it empowers young people with the resources, education, and opportunities necessary to thrive. When nations prioritize youth well-being through education, mental health support, and engagement in community, they can cultivate a generation that is capable of driving economic development and social cohesion, ultimately contributing to a prosperous society.
What are the global trends observed in youth flourishing based on recent studies?
Recent studies, like the Global Flourishing Study, reveal troubling trends in youth flourishing, showing that many Western nations, including the U.S., report lower levels of well-being among youth compared to older adults. This shift indicates that while youth may lack immediate satisfaction and support, factors like strong familial relationships and community connections can enhance their flourishing.
Why do middle-income countries perform better in youth flourishing compared to wealthier nations?
Middle-income countries often outperform wealthier nations in youth flourishing rankings because they may prioritize relationships and community engagement over material wealth. Wealth alone does not guarantee higher levels of well-being; instead, social connections and a sense of purpose frequently found in these nations contribute significantly to a richer, more satisfying life for youth.
How does economic development affect youth well-being and flourishing?
Economic development can positively impact youth well-being by increasing access to resources and opportunities; however, it can also lead to neglect of the social and spiritual dimensions of flourishing. As economies grow, it’s essential to balance financial success with nurturing relationships, purpose, and community to ensure comprehensive youth development.
What is the significance of childhood experiences on youth flourishing?
Childhood experiences play a critical role in shaping youth flourishing. Positive relationships with parents, good health, and supportive environments foster resilience and well-being in young people. These foundational experiences are linked to better flourishing outcomes in adulthood, making early investment in youth essential for long-term societal health.
What can be done to improve youth flourishing in economically developing nations?
To enhance youth flourishing in economically developing nations, strategies should focus on bolstering education, mental health services, and community programs that promote social connections and support networks. Engaging youth in meaningful activities and providing them with resources for personal and professional growth can also foster a flourishing environment.
How do cultural factors influence youth flourishing globally?
Cultural factors greatly influence youth flourishing, as different societies prioritize varying aspects of well-being, such as social relationships, education, and spiritual practices. Understanding these cultural nuances is essential for tailoring interventions that effectively promote youth well-being and flourishing across diverse global contexts.
| Key Points |
|---|
| A major global study shows the relationship between wealth and youth well-being is complex. |
| Middle-income countries outperform wealthy nations in youth flourishing, suggesting wealth is not the sole determinant of well-being. |
| The study indicates troubling trends for youth flourishing in Wealthy nations, particularly in the U.S. |
| Respondents identified health, happiness, relationships, and spiritual well-being as crucial variables in assessing flourishing. |
| Quality of family relationships and attending religious services positively impact adult flourishing regardless of economic status. |
Summary
Youth flourishing is a critical concern as recent studies reveal significant disparities in well-being among young individuals, particularly in affluent nations like the U.S. While economic status plays a role, the findings from a comprehensive global study emphasize that factors such as relationships, health, and spiritual engagement are equally, if not more, important for enhancing the flourishing of youth. It is essential for policymakers and society at large to prioritize these aspects to foster an environment that truly supports the growth and happiness of our youth.

Global Health Leadership: Gawande’s Call to Action
Global health leadership is essential to tackling the multifaceted challenges that plague our interconnected world. Renowned surgeon and author Atul Gawande highlights the critical point that the dismantling of USAID has left a gaping void in global health initiatives, jeopardizing crucial public health infrastructure worldwide. With reduced healthcare funding and staff, many effective programs targeting diseases like HIV, tuberculosis, and malaria face dire consequences. Gawande warns that while it may feel too late to restore the past glory of USAID, concerted efforts can still salvage essential health and science services. As future leaders in healthcare and medicine emerge, the importance of robust and resilient public health systems cannot be overstated, making global health leadership more pivotal than ever before.
In the realm of international health, the role of effective governance and strategic vision emerges as a cornerstone of sustainable wellness initiatives. Facing unprecedented challenges, the absence of strong public health leadership creates vulnerabilities that can reverberate across nations. Thought leaders like Atul Gawande stress the necessity of rebuilding and investing in foundational health frameworks, particularly in light of recent setbacks to organizations like USAID. By focusing on global health strategies that bridge funding gaps and bolster cooperative efforts, stakeholders can work to enhance health metrics worldwide. The urgency for a renewed commitment to healthcare leadership and collaborative global health efforts has never been more apparent.
The Impact of USAID on Global Health Initiatives
The United States Agency for International Development (USAID) has long been a cornerstone of global health initiatives, establishing programs that address pressing health concerns worldwide. Under the leadership of individuals like Atul Gawande, the agency has been able to effectively allocate resources toward combating infectious diseases, enhancing maternal and child health, and strengthening public health infrastructures in vulnerable regions. However, the recent cuts to USAID’s funding and operations have raised serious concerns about the future of these critical health programs, which have been instrumental in improving outcomes for millions.
Gawande’s remarks highlight the agency’s achievements, such as significantly reducing emergency response times to disease outbreaks and increasing vaccination rates in developing countries. The dismantling of its programs has not only jeopardized past successes but has also set back progress in global health by limiting access to essential healthcare services. This unfortunate trend raises the question of how the international community, including countries that may step into leadership roles, will respond to this crucial health void.
Strengthening Public Health Infrastructure Globally
Public health infrastructure is vital for the effective delivery of health services and for preparing for health emergencies. Gawande’s role at USAID exemplified how focused leadership can bolster global health efforts. He emphasized the importance of sustained funding and support for health programs, which leverage existing networks and local knowledge to improve public health outcomes. Organizations like USAID have historically played a significant role in this context by enabling countries to develop robust health systems capable of addressing both current and future challenges.
The consequences of neglecting public health infrastructure are profound. Countries with weakened health systems face increased vulnerability to outbreaks of diseases, which can lead to widespread health crises. Gawande’s commitment to fostering stronger health infrastructures through innovative financing and technical assistance underscores the need for re-engagement in global health initiatives, reminding us all that comprehensive care requires not just immediate solutions but also long-term investments.
The Role of Healthcare Funding in Global Health Leadership
Healthcare funding is a critical component of maintaining and advancing the effectiveness of global health initiatives. The recent cuts to USAID reflect a troubling trend in healthcare funding, one that threatens the operational capabilities of organizations that have historically provided vital health services across the globe. For instance, without adequate funding, programs that target diseases like HIV, tuberculosis, and malaria may falter, leaving millions without necessary treatments and preventative measures.
As Atul Gawande noted, the legacy of USAID’s healthcare funding has had a lasting impact on global health leadership. Investing in healthcare not only enriches individual lives but also enhances the overall health security of nations. By providing reliable support and funding for health initiatives, the U.S. has been able to assert itself as a global leader in health. The challenge now lies in rallying both public and private entities to recommit to healthcare funding, ensuring that the successes achieved over the years are not undone.
Atul Gawande: Vision for Future Global Health
Atul Gawande, with his vast expertise and leadership experience, envisions a more robust role for the U.S. in global health initiatives. Throughout his career, he has championed scientific advancement and the integration of effective public health measures. Despite setbacks, Gawande remains hopeful that with renewed focus and investment, the U.S. can regain its position as a leader in global health. His insights encourage a re-evaluation of current strategies and a re-engagement with the global health community to address existing challenges.
His tenure at USAID allowed him to witness the profound impact of dedicated health initiatives firsthand. Gawande’s message is clear: the future of global health depends on collaborative efforts, innovative solutions, and a firm commitment to public health infrastructure. As nations look to fill the leadership void left by the U.S., Gawande emphasizes that existing talent and expertise can guide future endeavors, shaping a healthier world for all.
The Importance of Science and Medicine in Global Health
Atul Gawande’s reflections on his experience at USAID point to a crucial truth: science and medicine are the driving forces behind effective global health strategies. Maintaining a strong commitment to scientific research is essential in developing evidence-based policies that address pressing health issues. The challenges posed by infectious diseases, maternal health, and childhood mortality are only surmountable through continuous investment in scientific research and medical innovation.
Gawande also spoke about how research funding, particularly in entities like the National Institutes of Health and the Centers for Disease Control, is pivotal for ongoing discoveries that inform public health initiatives. The intersection of science and medicine is where solutions are born, and as we face new health threats, the need for a united front in scientific inquiry becomes more essential than ever.
Future of Global Health Initiatives Post-USAID Cuts
The future of global health initiatives is uncertain following significant cuts to USAID’s operations. These changes not only diminish the agency’s capacity to respond to health crises but also raise concerns about the sustainability of the programs that have historically provided crucial healthcare services worldwide. The cuts send a strong message about prioritization in health funding, potentially diminishing the U.S. role as a leader in global health.
However, Gawande’s remarks serve as a rallying cry for the importance of these initiatives. While other countries may assume leadership roles, the value of U.S. contributions to health programs remains significant. The challenge now is to cultivate partnerships and collaborations that can fill these gaps, ensuring that the essential work of promoting health and preventing disease continues unabated.
Collaboration Among Nations in Global Health Efforts
The emphasis on collaboration in global health efforts has never been more critical. Atul Gawande’s leadership experiences demonstrate that working together with multiple stakeholders—including governments, nonprofits, and private sectors—can amplify health endeavors and maximize the impact of financial contributions. A collaborative approach allows for the sharing of resources, expertise, and innovative practices that can effectively address global health challenges.
As the world grapples with health disparities exacerbated by recent political changes, focusing on building alliances becomes paramount. Countries with emerging healthcare systems can benefit immensely from the lessons learned by veterans like the U.S. in integrating science and healthcare funding to enhance public health outcomes. By fostering a spirit of cooperation and mutual support, global health efforts can become more resilient and sustainable.
Addressing Challenges in Global Health Leadership
The challenges facing global health leadership in light of current political environments cannot be underestimated. With significant cuts to important initiatives and agencies like USAID, there is a need for a proactive strategy among global leaders to ensure that health continues to be a pressing priority. Atul Gawande’s insights remind us that the existing public health infrastructure needs support, and that a robust global response is required to combat the threats posed by diseases.
Moreover, Gawande warns that as traditional leadership roles falter, the onus will be on emerging nations to take charge. This transition could lead to exciting opportunities for new leaders to innovate and drive change in how healthcare is funded and delivered. However, maintaining momentum from established programs will require a commitment from all nations to protect and enhance healthcare initiatives globally.
The Intersection of Local and Global Health
Understanding the intersection of local and global health is essential in crafting successful health policies. Gawande illustrated how initiatives funded by organizations like USAID are not just beneficial on a global scale but have real, tangible impacts on local communities. By addressing health challenges in a local context, these global health programs help to build more resilient public health systems that benefit individuals and communities.
At the same time, the lessons learned from local health challenges have the potential to inform global health strategies. By recognizing how various local innovations can enhance public health infrastructure, countries can apply these solutions on a broader scale. The interplay between local and global responses is paramount to building a sustainable future for health, as Gawande emphasizes in his ongoing commitment to the field.
Frequently Asked Questions
What is the role of USAID in global health leadership?
USAID plays a crucial role in global health leadership by funding and implementing health initiatives worldwide. It has led programs that improve public health infrastructure, combat diseases like HIV, tuberculosis, and malaria, and enhance emergency response times during outbreaks, significantly contributing to better health outcomes for millions.
How did Atul Gawande contribute to global health initiatives during his time at USAID?
As head of USAID’s Bureau for Global Health, Atul Gawande oversaw significant global health initiatives that included reducing maternal and childhood mortality rates, improving treatment protocols, and establishing a network for rapid disease surveillance. His leadership emphasized technical assistance to elevate vaccination rates and health service delivery effectively.
What are some challenges faced by global health leadership in the US?
Challenges to US global health leadership include budget cuts, the dismantling of effective programs, and reduced healthcare funding that undermines essential global health initiatives. The recent freeze on research funding has also threatened critical partnerships and advancements in public health infrastructure.
Why is public health infrastructure important for global health leadership?
Public health infrastructure is vital for global health leadership as it supports disease prevention, healthcare access, and effective health responses during crises. A strong infrastructure enables timely interventions, comprehensive health strategies, and the sustainability of health initiatives across nations.
What is the future of global health leadership in the wake of recent funding issues?
The future of global health leadership may shift as funding issues persist. While the US has historically played a leading role, other countries may step in to fill the void. Continued commitment to science and public health by professionals like Atul Gawande will be essential to maintain progress in global health.
How do healthcare funding cuts affect global health initiatives?
Healthcare funding cuts can severely affect global health initiatives by limiting resources available for disease prevention, treatment programs, and research. Such cuts have led to the termination of essential services, which can increase mortality rates and diminish the effectiveness of established global health strategies.
What lessons can be learned from Atul Gawande’s experience with USAID?
Lessons from Atul Gawande’s experience at USAID highlight the importance of sustaining healthcare funding, maintaining qualified personnel, and ensuring robust public health infrastructure. His emphasis on follow-through reiterates that successful global health leadership relies not only on solutions but also on their effective implementation and scale.
| Key Point | Details |
|---|---|
| Gawande’s Insights on USAID | He discussed the detrimental effects of the Trump administration’s cuts to USAID, emphasizing the loss of programs crucial for global health. |
| Impact of Funding Cuts | The cuts have led to significant damage affecting millions globally and jeopardized ongoing health programs, including crucial research at Harvard. |
| Urgency for Action | Gawande stressed it’s not too late to save health and science infrastructure, calling for commitment from health leaders and students. |
| Success Stories from USAID | USAID had previously improved global health metrics significantly, reducing emergency response times and preventing maternal and childhood deaths. |
| Future of Global Health Leadership | Despite challenges, Gawande expressed hope in the leadership role the U.S. can still adopt in global health amidst uncertainties. |
Summary
Global health leadership is at a pivotal crossroads as highlighted by Atul Gawande. His observations on the dismantling of critical healthcare agencies underlines the urgency for a renewed commitment to international health initiatives. Despite the setbacks, Gawande inspires hope for the future, encouraging emerging leaders in health to play a vital role in ensuring that vital healthcare infrastructure is not only maintained but enhanced. As we move forward, the importance of sustained leadership in global health cannot be overstated.

Medical Research Funding: Ensuring Patient Safety Amid Cuts
Medical research funding is vital for advancing scientific understanding and ensuring patient safety in clinical studies. Without adequate financial support, the impact of funding on research becomes detrimental, disrupting crucial oversight mechanisms that protect participants. Institutions like Harvard have faced significant challenges due to a freeze in federal grants, which highlights the essential role of funding in facilitating Institutional Review Board (IRB) functions. These boards are responsible for safeguarding patient protection in research, ensuring that studies adhere to ethical practices and regulations. As a result, the effects of NIH funding and its consequences on the safety and effectiveness of medical investigations cannot be overstated.
Financial support for healthcare research, often referred to as medical research financing, plays a pivotal role in shaping the landscape of clinical trials. When there is a lack of investment, the intricacies involved in maintaining participant safety and ethical oversight can be severely compromised. Resources from funding agencies, such as the NIH, underscore their importance and effectiveness in upholding participant welfare and ensuring rigorous review processes through IRB oversight. Moreover, the ramifications of halted funding ripple through the research community, potentially eroding public trust and hindering progress in medical innovations that benefit countless patients. In essence, the availability of research funding is deeply intertwined with the integrity and success of scientific endeavors in the health sector.
The Importance of Medical Research Funding in Patient Safety
Medical research funding is crucial for advancing healthcare and improving patient safety. Funding from organizations like the National Institutes of Health (NIH) ensures that necessary resources are available for conducting thorough clinical studies. These studies, thoroughly vetted by Institutional Review Boards (IRBs), investigate the potential benefits and risks associated with new therapies, medications, and medical devices. When funding is stable, research initiatives can move forward efficiently, allowing for the continued evaluation of patient protection measures and safety protocols within the medical community.
However, disruptions in funding, such as the recent halt of $2 billion in federal research grants to institutions like Harvard, pose significant risks to patient safety. Not only do these funding cuts stall ongoing studies, but they also hinder the implementation of crucial safety measures that protect participants. The lack of resources can lead to delays in approving necessary trials or modifications to existing studies, ultimately affecting how effectively researchers can address potential adverse effects.
Impact of Funding Cancellations on Research and Ethics
Cancellations of medical research funding present a serious challenge to the ethical standards set by IRBs, which exist to protect the rights and welfare of research participants. When funding is removed, the comprehensive review processes that IRBs provide may struggle to maintain their thoroughness, leading to potential lapses in safety oversight. Research professionals rely on this funding to adhere to ethical practices; without it, both the integrity of research and the security of participants may be compromised.
Furthermore, the cancellation of funding can lead to a systemic breakdown in the collaborative networks that IRBs rely on to ensure comprehensive oversight across multiple sites. With the halt of funds, new institutions cannot join ongoing trials, which stifles innovation and the sharing of vital knowledge among researchers. The resulting fragmentation can heighten ethical concerns related to informed consent and patient safety while breeding mistrust within the communities that researchers aim to serve.
The Role of IRBs in Safeguarding Participants
Institutional Review Boards (IRBs) play a vital role in safeguarding research participants by ensuring that ethical standards are met throughout the lifecycle of medical studies. These boards are responsible for reviewing recruitment strategies, monitoring potential risks, and ensuring that informed consent processes are transparent and effective. The knowledge and oversight provided by IRBs become even more critical in the context of tight funding, where the potential for compromising participant welfare may increase without adequate fiscal resources.
Additionally, IRBs serve as educators for researchers, instilling best practices in protecting participants. By emphasizing ethical conduct and oversight, they foster an environment where patient protection is paramount, thereby reinforcing public trust in the research process. In light of funding challenges, IRBs must continue to advocate for stringent ethical standards to maintain the integrity of medical research and the safety of participants.
Evaluating the Historical Context of Medical Research Funding
To understand the pivotal role of funding in medical research, it is essential to consider historical events that have influenced current ethical guidelines. Historical abuses, such as the Tuskegee Syphilis Study and the inhumane treatment of participants at Willowbrook State School, have shaped the stringent requirements set forth by IRBs to ensure participant protection. These events underscore the necessity for well-funded oversight processes that monitor and facilitate ethical research practices.
The lessons learned from history emphasize the correlation between funding availability and protective measures for patients. A well-funded research environment enables institutions to implement comprehensive ethical frameworks and oversight mechanisms that have emerged since these dark chapters in medical history. As funding becomes increasingly variable, it remains vital that institutions prioritize the ethical review of research practices to safeguard the public’s trust and welfare.
Consequences of Research Funding Cuts on Innovation
Research funding cuts pose severe consequences for innovation in medical science and therapeutic development. A halt in financial support can mean that institutions and researchers are unable to explore promising avenues for treatment, particularly in urgent areas like Alzheimer’s disease or cancer therapies. With significant federal funding, researchers can tackle complex problems collaboratively, share insights, and accelerate the development of life-saving treatments. Unfortunately, without adequate funding, these crucial opportunities for innovation become significantly limited.
Moreover, the interplay between funding and collaborative initiatives is critical for advancing medical research. Systems like the SMART IRB, designed to streamline multi-site studies, heavily depend on consistent funding to operate effectively. The potential to support groundbreaking treatments diminishes when funding is cut, leading to increased delays in bringing new therapies to market. The broader implications of these cuts not only affect researchers but ultimately impact patient access to emerging medical advancements.
Protecting Patient Rights: The Financial Aspect
Patient rights and safety are intrinsically linked to the financial resources allocated for medical research. Funding from governmental and private entities is vital in upholding the standards that protect participants during clinical trials. Without adequate financial backing, the ability of IRBs and research institutions to monitor compliance with ethical guidelines may be significantly undermined, leading to increased risks for participants and diminished trust in the research process.
Furthermore, when financial resources are limited, institutions may struggle to implement best practices in terms of participant communication and education about their rights. Robust funding is necessary to support initiatives that inform participants of their rights and the potential risks and benefits involved in research. As a result, ensuring adequate funding for medical research is not merely a financial issue—it is fundamentally about safeguarding the dignity and welfare of those participating in clinical studies.
NIH Funding Effects on Collaborative Research
The effects of NIH funding on collaborative research initiatives cannot be overstated. NIH grants are often instrumental in driving forward multi-site studies that require coordinated oversight and resources across various institutions. This funding fosters an environment of collaboration, allowing researchers to share data, resources, and expertise effectively. Such collaboration is crucial in medical research, as it accelerates the pace at which new knowledge can be generated and implemented for patient care.
However, when NIH funding is lost or suspended, the collaborative spirit of research can suffer. Institutions may become isolated in their studies, leading to redundancies and inefficiencies that can hinder progress. The resulting fragmentation not only impairs the ability to conduct thorough investigations but can also influence how findings are disseminated and utilized in clinical practice, ultimately affecting patient care and treatment outcomes.
The Ethical Imperative of Funding in Medical Studies
Funding in medical studies is not just a bureaucratic necessity; it is an ethical imperative. Adequate funding ensures that studies adhere to rigorous ethical standards, thereby protecting participants and enhancing research quality. When researchers are assured of stable financial support, they can focus on designing robust studies with comprehensive safety measures, which directly contributes to the well-being of participants. IRBs play a crucial role in this system by evaluating the proposed research against ethical benchmarks, helping to ensure that patients are treated with respect and dignity.
Moreover, when funding is secure, researchers invest in the training and education required for all individuals involved in a study, fostering a culture of safety and ethical responsibility within research teams. This investment is essential for maintaining a high standard of ethical conduct in medical research, ultimately benefitting the public and advancing medical science. Therefore, reinforcing the importance of funding is indispensable to uphold the ethical foundations of medical research.
Public Trust and Research Funding Stability
Public trust is vital for the success of medical research, and funding stability plays a significant role in fostering this trust. When sufficient resources are allocated for ethical oversight, compliance, and protection of participants’ rights, the public is more likely to have confidence in the research process. Trust is further enhanced when stakeholders can see the tangible benefits of funded research through improved health outcomes and advances in medical practice.
Conversely, disruptions in funding can lead to public skepticism regarding the integrity of research. For instance, recent cuts to funding have raised concerns among potential participants about whether their safety and rights are adequately protected during studies. Therefore, maintaining a steady stream of funding is essential not only for the advancement of medical science but also for preserving the trust of patients and the communities impacted by research.
Frequently Asked Questions
What is the impact of funding on medical research and patient safety?
Funding plays a crucial role in medical research, significantly contributing to patient safety. Well-funded research allows for thorough oversight through Institutional Review Boards (IRBs), ensuring compliance with ethical guidelines. Without sufficient funding, oversight mechanisms may suffer, risking participant safety and research integrity.
How do NIH funding effects impact patient protection in research?
NIH funding affects patient protection by facilitating thorough review and oversight by IRBs. These boards ensure that studies comply with safety regulations, thereby safeguarding participants’ rights and welfare. Adequate NIH support is essential for maintaining robust patient protection in ongoing medical research.
What role do IRB functions play in ensuring safety in medical studies?
IRB functions are critical in ensuring safety in medical studies. They meticulously assess research proposals, evaluate risks, and ensure informed consent processes are in place. This oversight protects patients by preventing ethical breaches and fostering a trustworthy research environment.
How does the halt in funding disrupt the impact of funding on research?
A halt in funding disrupts the impact of funding on research by delaying studies and limiting the resources available for IRB oversight. This may hinder the commitment to ethical practices, ultimately affecting patient safety and community trust in medical research.
What is the relationship between the impact of funding on research and the safety of patients?
The relationship between the impact of funding on research and patient safety is direct; adequate funding ensures comprehensive oversight by IRBs, which is essential for protecting patient rights and welfare during clinical trials. Cutbacks in funding can compromise these protective measures.
| Key Points | Details |
|---|---|
| Impact of Funding Cuts | The Trump administration’s freeze of over $2 billion in federal research grants, including a stop-work order on SMART IRB, disrupts oversight of patient safety in research. |
| Role of IRBs | IRBs ensure the protection of research participants through review processes, informed consent, and oversight mechanisms. |
| Historical Context | Incidents like the Tuskegee study highlight the critical need for ethical oversight in medical research. |
| Consequences for Patients | Delays in studies and collaboration due to funding cuts can compromise participant safety and hinder medical breakthroughs. |
| Importance of Collaboration | SMART IRB was created to streamline collaboration among multiple research sites, enhancing efficiency and safety in medical studies. |
Summary
Medical research funding is crucial for ensuring the safety and rights of patients involved in clinical studies. The recent funding cuts have disrupted essential oversight mechanisms, such as the SMART IRB, leading to significant delays and potential risks to participant welfare. Without adequate funding, research institutions are unable to effectively collaborate, further jeopardizing public trust in the medical research enterprise. Investing in medical research funding is imperative to protect patients and promote ethical standards in research.

Vaping Cessation Medication: A New Hope for Teens
Vaping cessation medication is proving to be a crucial tool in the fight against nicotine addiction among young people. Recent studies indicate that young adults and teens who utilize FDA-approved options, such as varenicline, have significantly higher success rates when attempting to quit vaping. In fact, those taking this medication were shown to be more than three times more likely to overcome their vaping habits compared to those receiving standard behavioral counseling alone. As the prevalence of vaping continues to rise, particularly among teens, it becomes increasingly important to explore effective nicotine addiction treatment options that cater specifically to this vulnerable demographic. The promising results from recent clinical trials suggest that incorporating medication into cessation strategies could greatly enhance the ability of young adults to quit vaping for good.
The push to end nicotine dependency is gaining momentum with innovative quitting aids that target younger populations. Medications aimed at reducing the urge to vape, such as varenicline, which is already recognized for its effectiveness in adult smoking cessation, have now been adapted for young smokers. This shift reflects a growing acknowledgment of the challenges teens and young adults face when trying to break free from vaping habits. By demonstrating clear benefits, these pharmacological treatments align with existing behavioral support mechanisms, creating a powerful approach to combating teen vaping. As awareness of the health risks linked to vaping rises, these cessation resources are becoming essential in safeguarding the future of young nicotine users.
Understanding the Rise of Vaping in Teens
Vaping has become an increasingly popular trend among teens and young adults, leading to a significant public health concern. Recent statistics indicate that nearly a quarter of individuals aged 18 to 25 vaped in the past year, alongside a worrying 8% of high school students engaging in this habit. This dramatic rise in vaping correlates with the perception of vapes as safer alternatives to traditional cigarettes, despite containing harmful substances that can lead to nicotine addiction and other health risks. Parents and educators alike face the challenge of understanding and addressing this trend among youth, who often view vaping as a harmless, inconspicuous activity.
The implications of early nicotine exposure extend beyond immediate addiction; evidence suggests that it may also heighten vulnerability to future substance use disorders, including those involving more potent drugs. As young individuals often lack the necessary awareness about the health effects of vaping, it becomes critical for adults to engage in open discussions, educating them about the potential risks associated with nicotine and encouraging healthier choices. In light of the surge in vaping, it is imperative to foster a supportive environment for teens to seek help and guidance.
The Efficacy of Varenicline for Young Adults
Varenicline, an FDA-approved medication traditionally used for smoking cessation in adults, has shown promising results for young adults seeking to quit vaping. Recent clinical research conducted by Mass General Brigham revealed that participants aged 16 to 25 using varenicline had a success rate over three times higher than those who received only behavioral counseling, signifying a breakthrough in nicotine addiction treatment for teens and young adults. This finding underscores the necessity for exploring medication-based interventions as effective tools for combating nicotine dependence among vulnerable populations.
The study not only demonstrated the effectiveness of varenicline in facilitating vaping cessation but also showcased its safety profile. Participants who successfully quit vaping did not revert to cigarette smoking, highlighting the medication’s capacity to assist young adults in overcoming their addiction without prompting alternative harmful behaviors. This paves the way for the wider adoption of varenicline in treatment plans that aim to help teens and young adults reclaim their health and well-being.
Behavioral Counseling and Vaping Cessation
While varenicline proves effective in supporting vaping cessation, behavioral counseling remains a considerable component of comprehensive treatment strategies. In the clinical trial, participants received weekly behavioral counseling in conjunction with medication, emphasizing the importance of addressing the psychological and social factors inherent in nicotine addiction. Behavioral counseling offers young individuals the tools to confront triggers and develop healthier coping mechanisms, laying a robust foundation for lasting recovery from vaping and nicotine dependence.
Moreover, integrating behavioral counseling with pharmacological treatment creates a holistic approach to quitting vaping. This combination not only enhances success rates but also empowers teens and young adults with the strategies they need to avoid relapse. Such dual-faceted support can be instrumental in breaking the cycle of nicotine addiction and ensuring that young people move towards a healthier, vape-free lifestyle.
Long-Term Effects of Vaping on Youth
The long-term effects of vaping on youth are still under investigation; however, emerging research indicates significant risks associated with early exposure to nicotine. Teens who start vaping may develop a strong addiction, which can lead to further substance use issues later in life. Understanding the long-term consequences is crucial for health professionals, educators, and policymakers as they work to mitigate the repercussions of this growing epidemic within youth populations.
As public health campaigns begin to address the risks associated with vaping, it becomes increasingly important to provide resources tailored to the unique experiences and challenges faced by adolescents. By educating young people on the potential dangers of vaping, including cognitive and emotional development impacts, stakeholders can significantly contribute to prevention efforts aimed at reducing nicotine addiction in teens and young adults.
The Role of Support Services in Vaping Cessation
Support services such as text support programs have emerged as valuable resources for individuals seeking to quit vaping. Programs like ‘This is Quitting’ offer young adults instant access to information, encouragement, and tips designed to facilitate their cessation journey. These services play a crucial role in providing the additional support needed to complement medication like varenicline, enhancing the chances of quitting successfully.
Additionally, support services can foster a sense of community among young people facing similar struggles with vaping. By connecting individuals with others who are also attempting to quit, these programs can help combat feelings of isolation and encourage accountability. This community-driven support can be instrumental in maintaining motivation and perseverance throughout the challenging process of quitting vaping.
Preventive Measures Against Vaping in Schools
Implementing preventive measures within educational settings is essential to combat the growing trend of vaping among students. Educational institutions are increasingly adopting programs to raise awareness about the risks of vaping, educating students on nicotine addiction, and providing resources for those seeking to quit. These preventative strategies serve not only to inform students but also create a supportive environment where discussions about vaping are normalized and encouraged.
Schools can also establish policies that address the availability and use of vaping products on campus, which can contribute to a broader culture of health. By fostering a proactive stance against vaping, educators can take significant steps towards reducing its prevalence among teens. Collaborating with parents, health professionals, and community organizations to create comprehensive prevention programs can further enhance these efforts, addressing vaping both inside and outside of school.
Research and Development in Vaping Cessation Treatments
Research on vaping cessation treatments is evolving, revealing critical insights into effective strategies for helping young individuals quit. Recent studies have begun to explore the efficacy of existing medications, such as varenicline, specifically within the adolescent population. By examining how these medications can be adapted for younger audiences, researchers aim to improve treatment plans tailored to the unique needs of teens and young adults facing nicotine addiction.
Additionally, innovation within the field of nicotine addiction treatment is crucial for developing new interventions that resonate with the younger demographic. Research initiatives focusing on both pharmacological and behavioral strategies will enhance the understanding of how best to support teens in breaking free from nicotine dependence. Continued investment in research provides hope for more effective treatments that can address the urgent public health issue of vaping among youth.
The Importance of Parental Involvement in Vaping Cessation
Parental involvement plays a vital role in shaping teens’ attitudes towards vaping and their likelihood of quitting. Open communication about the dangers of vaping, paired with support for cessation efforts, can significantly impact a young person’s success in overcoming nicotine addiction. Parents are often the first line of defense in educating their children and providing the guidance necessary for making healthier decisions.
Furthermore, parents can act as role models by demonstrating healthy behaviors and openly discussing their own experiences with substance use. Encouraging an environment that values health and well-being can motivate teens to recognize the need for change and actively pursue quitting. When parents engage in their children’s lives regarding vaping, they foster a collaborative approach where teens feel supported in their efforts to quit.
Future Directions in Vaping Research and Policy
Looking ahead, ongoing research and policy development will be essential in addressing the vaping epidemic among young people. Policymakers need to stay informed on the evolving landscape of e-cigarettes and their impact on public health. Comprehensive regulations that restrict access and promote education about the dangers of vaping are necessary to mitigate its prevalence among adolescents. This could involve stricter advertising regulations, age restrictions, and educational mandates within schools.
Additionally, collaboration between researchers, healthcare providers, and policymakers will be crucial in developing targeted interventions that can effectively reduce youth vaping rates. As the understanding of vaping and its dangers evolves, ensuring that policies are adaptable and evidence-based will be key to safeguarding public health. By prioritizing research and policy initiatives, society can take meaningful steps towards addressing the vaping crisis among teens and young adults.
Frequently Asked Questions
What is vaping cessation medication and how does it help to quit vaping?
Vaping cessation medication, like varenicline, is designed to help individuals stop using nicotine products, including e-cigarettes. This FDA-approved smoking cessation pill has shown effectiveness in clinical trials, particularly among adolescents and young adults, providing a medical option to support quitting vaping.
Is varenicline safe for young adults trying to quit vaping?
Yes, varenicline is considered safe for young adults aged 16 to 25 who want to quit vaping. Clinical studies have shown that it not only helps individuals achieve higher success rates in quitting but also does not lead to increased smoking among those quitting vaping.
How effective is varenicline for teens and young adults in quitting vaping?
Clinical trials have shown that teens and young adults using varenicline for vaping cessation had over three times higher success rates in quitting compared to those using placebo. At 12 weeks, more than half of the participants using varenicline successfully stopped vaping.
Can FDA-approved smoking cessation methods help with nicotine addiction treatment for teens?
Yes, FDA-approved smoking cessation methods like varenicline are effective in treating nicotine addiction among teens. Recent studies highlight its efficacy and safety, making it a viable option for adolescents struggling with vaping addiction.
What alternatives exist to quit vaping besides medication?
While vaping cessation medication such as varenicline is highly effective, behavioral counseling and support groups can also assist individuals in quitting vaping. Combining medication with counseling, like weekly sessions and text support, has shown to enhance success rates significantly.
What demographic is most affected by vaping addiction?
Vaping addiction primarily affects teens and young adults, with studies showing that about a quarter of individuals aged 18 to 25 vaped in 2023, highlighting the urgent need for effective cessation strategies targeted at this age group.
What are the benefits of using varenicline for young adults who vape?
Using varenicline as a vaping cessation medication can significantly increase the chances of quitting. Benefits include a higher likelihood of success compared to behavioral therapy alone, and safety indicated by research, making it an effective choice for combating nicotine addiction.
How soon can one expect results from vaping cessation medication like varenicline?
Individuals using varenicline for vaping cessation can expect significant results within the first 12 weeks, with many experiencing improved quitting success rates compared to those not using the medication.
Why is it important to explore medication options for quitting vaping among young people?
It is crucial to explore medication options for quitting vaping among young people due to the rising rates of nicotine addiction and the potential long-term health risks associated with early exposure to nicotine, making effective treatment pathways essential.
What role does behavioral counseling play alongside vaping cessation medication?
Behavioral counseling enhances the effectiveness of vaping cessation medication like varenicline by providing support and strategies to address the behavioral aspects of addiction, leading to better overall outcomes in quitting.
| Key Point | Details |
|---|---|
| FDA-Approved Medication | Varenicline is an FDA-approved smoking cessation pill that can be prescribed to individuals aged 16 to 25. |
| Clinical Trial Success | Teens and young adults using varenicline were three times more likely to quit vaping compared to those on placebo. |
| Study Results | At 12 weeks, 51% of varenicline users stopped vaping; only 14% of placebo users did. |
| Safety of Varenicline | No nicotine vape users who switched to varenicline turned to cigarette smoking, indicating safety. |
| Need for Continued Research | Further research is needed to explore other treatments and to include younger users. |
Summary
Vaping cessation medication, particularly varenicline, plays a pivotal role in supporting teens and young adults in quitting vaping effectively. This FDA-approved pill has been shown to significantly increase the success rates of quitting among users in clinical trials, especially when combined with behavioral counseling. The promising results underscore the urgent need for accessible and effective treatment options to combat nicotine addiction in younger populations.

Bile Imbalance Linked to Liver Cancer: Key Insights Revealed
Bile imbalance is emerging as a significant factor in the development of liver cancer, particularly hepatocellular carcinoma (HCC), the most prevalent type of liver malignancy. Recent studies highlight how irregularities in bile acid metabolism can lead to liver diseases that compromise health and increase the risk of cancer. Understanding the role of bile acids, which are produced by the liver to help digest fats, is crucial for developing effective liver cancer treatment strategies. Research has unveiled a key molecular switch implicated in this process, providing new insights into the FXR receptor’s functionality in maintaining bile equilibrium. As we delve deeper into the interplay between bile acids and liver disease, it becomes clear that managing bile imbalance may offer novel therapeutic avenues for combatting liver cancer.
Exploring the complex relationship between bile constituents and hepatic malignancies reveals an urgent need for awareness regarding bile acid dysregulation in liver disorders. Hepatocellular carcinoma (HCC) has gained attention as studies focus on the metabolic roles of bile acids and their relationship with liver health. The investigation into FXR activation underscores its potential as a therapeutic target in liver disease management. By comprehensively examining the influences of bile acid turnover on liver functionality, researchers aim to better understand the mechanisms leading to liver cancers. This emerging area holds promise for innovative interventions that could significantly alter the course of liver cancer treatment.
Understanding the Role of Bile Acids in Liver Health
Bile acids, produced by the liver, are crucial for proper digestion and absorption of dietary fats. These acids function as detergents, emulsifying fats into smaller droplets, which enhances their absorption in the intestines. However, emerging research suggests that bile acids play a significant role beyond digestion; they act as signaling molecules that regulate various metabolic processes. A balanced bile acid metabolism is essential for maintaining liver health, and any imbalance can lead to severe complications, including liver disease and cancer.
The liver’s ability to produce bile is tightly regulated, and disturbances in this regulation can result in the accumulation of bile acids in the liver, leading to toxicity and inflammation. As detailed in a recent study, the repressor function of the YAP protein in bile acid metabolism can disrupt this balance, promoting conditions favorable for hepatocellular carcinoma (HCC). Thus, understanding bile acid dynamics is crucial for developing therapeutic strategies for liver conditions, highlighting the importance of maintaining healthy bile balance.
Bile Imbalance and Its Link to Liver Cancer
Recent studies indicate a troubling link between bile acid imbalance and the onset of liver cancer, specifically hepatocellular carcinoma (HCC). The overproduction of bile acids, driven by disruptions in the signaling pathways involving molecules like the FXR receptor and YAP, contributes to liver fibrosis and inflammation, which are precursors to cancer. It is vital to recognize that the liver’s response to bile acid levels can dictate the progression towards malignancy, emphasizing the need for targeted treatment interventions that restore this balance.
Addressing bile acid imbalance could prove to be a critical factor in liver cancer treatment strategies. The study led by Yingzi Yang highlights potential pharmacological approaches that can enhance FXR function to combat bile acid overproduction. By modulating bile acid metabolism, researchers are paving the way for innovative treatments that may not only prevent liver cancer but also reverse some of the damage caused by chronic liver disease, signifying a hopeful advancement in oncology.
The Hepato-YAP Signaling Pathway in Liver Disease
The Hippo signaling pathway, particularly its effector YAP, has gained prominence in cancer research due to its role in regulating cell growth and development. In liver diseases, including hepatocellular carcinoma, YAP’s influence extends to bile acid metabolism. YAP’s unexpected role as a repressor of FXR function signifies a complex interplay between cell signaling and metabolic regulation, making it a crucial target for therapeutic intervention in liver cancer treatment.
Understanding how YAP regulates bile acid synthesis and degradation offers new insight into the pathophysiology of liver disease. With increased YAP activity leading to bile acid accumulation, researchers are exploring how to inhibit YAP or activate FXR to restore metabolic homeostasis within the liver. These insights not only reveal new targets for liver cancer therapies but also illustrate the intricate relationship between metabolic disturbances and tumorigenesis in the liver.
Therapeutic Innovations in Bile Acid Metabolism
Advancements in understanding bile acid metabolism are paving the way for new therapeutic options for liver diseases, especially hepatocellular carcinoma. Recent studies suggest that enhancing the function of the FXR receptor could mitigate the harmful effects of bile acid accumulation in the liver. By stimulating FXR, it may be possible to rectify bile acid imbalances, thereby reducing inflammation and preventing cancer progression.
Additionally, discovering proteins involved in bile acid export, like BSEP, can serve as another clinical target. Increasing the expression of such transport proteins could facilitate excess bile acid excretion, alleviating liver damage. These innovative strategies underscore the potential for developing drugs that specifically address bile acid dysregulation, creating a multifaceted approach to liver cancer treatment.
The Future of Liver Cancer Treatments
As researchers delve deeper into the biochemical pathways affecting liver health, the implication for liver cancer treatments is profound. The findings surrounding bile acid metabolism and its regulation by the FXR receptor and YAP provide a roadmap for developing personalized therapies. By shifting focus from traditional cancer therapies to those that target metabolic pathways, the future of liver cancer treatment may become more effective and less toxic.
Such advancements stem from a comprehensive understanding of liver cancer biology, which emphasizes prevention through the management of bile acid imbalance. As new interventions, such as FXR agonists, are explored in clinical settings, they hold the promise of transforming liver cancer prognosis, emphasizing the critical need for continued research in this vital area of health.
The Impact of Nutrition on Bile Acid Metabolism
Nutrition plays a pivotal role in regulating bile acid production and metabolism. Diets high in fats can stimulate the liver to produce more bile acids, which could lead to an imbalance if not managed properly. This imbalance can result in toxic bile acid accumulation, triggering cellular damage and inflammation that may predispose individuals to liver diseases, including hepatocellular carcinoma. Thus, dietary choices significantly influence bile acid dynamics and overall liver health.
Moreover, incorporating foods that promote healthy bile acid metabolism, such as omega-3 fatty acids, fruits, and vegetables, may be beneficial. These dietary components can help modulate bile acid synthesis and support liver function, thereby reducing the risk of liver cancer. Understanding the nutritional aspects of bile acid metabolism presents viable strategies for disease prevention and management.
Research Developments in Liver Cancer Prevention
Ongoing research into liver cancer prevention strategies emphasizes the importance of understanding bile acid metabolism and its connection with obesity and metabolic disorders. As studies reveal the mechanisms linking bile imbalance and liver disease, researchers are able to identify risk factors and promote lifestyle interventions that could prevent the onset of hepatocellular carcinoma. Public health campaigns focusing on liver health may emerge as essential tools in combating liver cancer.
Additionally, collaboration between researchers, healthcare providers, and the community will be critical in disseminating findings regarding bile acids and liver cancer. Early detection methods, screening practices, and awareness programs may integrate new insights from studies on bile imbalance to enhance liver cancer prevention efforts, ultimately saving lives by addressing the disease before it progresses.
Clinical Trials and Emerging Therapies for Liver Cancer
Clinical trials exploring novel therapies targeting bile acid metabolism are gaining traction in the fight against liver cancer. With scientists investigating drugs that modulate the FXR receptor and its downstream effects on bile acid signaling, a new class of treatments may soon be at the forefront of hepatic care. These innovative therapies not only aim to reduce cancer risk but also seek to improve liver health overall, offering hope to patients affected by liver diseases.
As significant numbers of patients are enrolled in trials assessing the efficacy of these emerging therapies, their potential implications for liver cancer treatment will be critically monitored. The ongoing studies will provide pivotal data that could lead to breakthroughs in how liver cancer is managed, demonstrating the importance of research in understanding the complex interactions between bile acids and liver health.
The Role of Genetic Factors in Bile Acid Dynamics
Genetic predispositions can significantly impact bile acid metabolism, influencing an individual’s risk of developing liver diseases and cancers. Variations in genes responsible for bile acid transport and synthesis can lead to imbalances that may contribute to liver injury and inflammation. Research into these genetic factors is essential for identifying individuals at higher risk for hepatocellular carcinoma.
By deciphering the genetic underpinnings of bile acid metabolism, healthcare professionals may tailor prevention and treatment strategies based on a person’s genetic makeup. Personalized medicine approaches could vastly improve the outcomes for individuals facing liver cancer, highlighting the critical intersection of genetics, metabolism, and oncology in contemporary health research.
Frequently Asked Questions
How does bile imbalance contribute to liver cancer?
Bile imbalance is critical in the development of liver cancer, especially hepatocellular carcinoma (HCC). When bile acids are produced in excess or are improperly regulated, they can cause liver inflammation and fibrosis, leading to cellular damage and cancerous changes in liver tissue.
What role do bile acids play in liver disease and cancer?
Bile acids are not only essential for digestion but also act in regulating metabolic processes. Disruptions in bile acid metabolism can lead to liver disease. Studies suggest that an imbalance may contribute to the development of liver cancer by promoting inflammation and regenerating problematic signaling pathways.
What is the connection between FXR receptor and bile acid metabolism in liver cancer?
The FXR (Farnesoid X receptor) plays a vital role in bile acid homeostasis. In liver cancer, the activation of YAP inhibits FXR function, leading to bile acid overproduction and subsequent liver damage. Therapeutic strategies that enhance FXR activity could potentially mitigate the progression of liver cancer.
Are there potential treatments for liver cancer linked to bile imbalance?
Yes, targeting bile acid metabolism through pharmacological interventions that stimulate FXR could provide new avenues for liver cancer treatment. Enhancing FXR function or promoting bile acid excretion may disrupt the cycle of damage, reducing the risk of developing HCC.
What findings were highlighted in the HCC study regarding bile acids?
The recent HCC study identified a key molecular switch that regulates bile acid production. It revealed that YAP, which is often linked to tumor growth, paradoxically acts as a repressor of FXR, leading to bile acid dysregulation and potential liver cancer development.
What is the significance of the Hippo/YAP pathway in liver cancer and bile imbalance?
The Hippo/YAP pathway is crucial for regulating cell growth and its disruption can lead to cancer progression. In the context of liver cancer, YAP activation interferes with bile acid metabolism, suggesting it plays a significant role in the connection between bile imbalance and liver cancer.
How can understanding bile acid metabolism impact liver cancer treatment?
Understanding bile acid metabolism is essential as it opens new therapeutic pathways. By targeting the molecular interactions involving bile acids and receptors like FXR, researchers may develop innovative treatments that not only manage liver diseases but also prevent the progression to liver cancer.
| Key Points | Details |
|---|---|
| Bile Imbalance and Liver Cancer | Bile acid imbalance can trigger liver diseases, particularly hepatocellular carcinoma (HCC), the most prevalent form of liver cancer. |
| Study Insights | A critical molecular switch regulating bile acids has been identified, with implications for liver cancer treatment. |
| Role of Bile | Bile acids help digest fats and regulate metabolic processes; disruption leads to liver injury and cancer. |
| YAP/FXR Pathway | YAP inhibits FXR, a vital sensor for bile acid homeostasis, leading to bile acid overproduction and liver cancer. |
| Potential Treatments | Activating FXR or promoting bile acid excretion may block the cancer progression cycle. |
| Funding and Research Background | Research was supported by NIH and NCI, focusing on cell signaling in liver biology and cancer. |
Summary
Bile imbalance linked to liver cancer has emerged as a significant concern in understanding and developing treatment strategies for hepatocellular carcinoma (HCC). Recent research highlights the critical role of bile acids in liver health, demonstrating that their disruption can lead to serious liver diseases, including HCC. The identification of a key molecular switch, such as the YAP protein’s interaction with the FXR regulatory pathway, opens new avenues for potential therapies aiming to restore normal bile acid metabolism. This research emphasizes the need for continued exploration into how bile imbalance affects liver cancer progression, potentially paving the way for innovative pharmacological interventions.