Medical Research Funding: How Cuts Affect Patient Safety
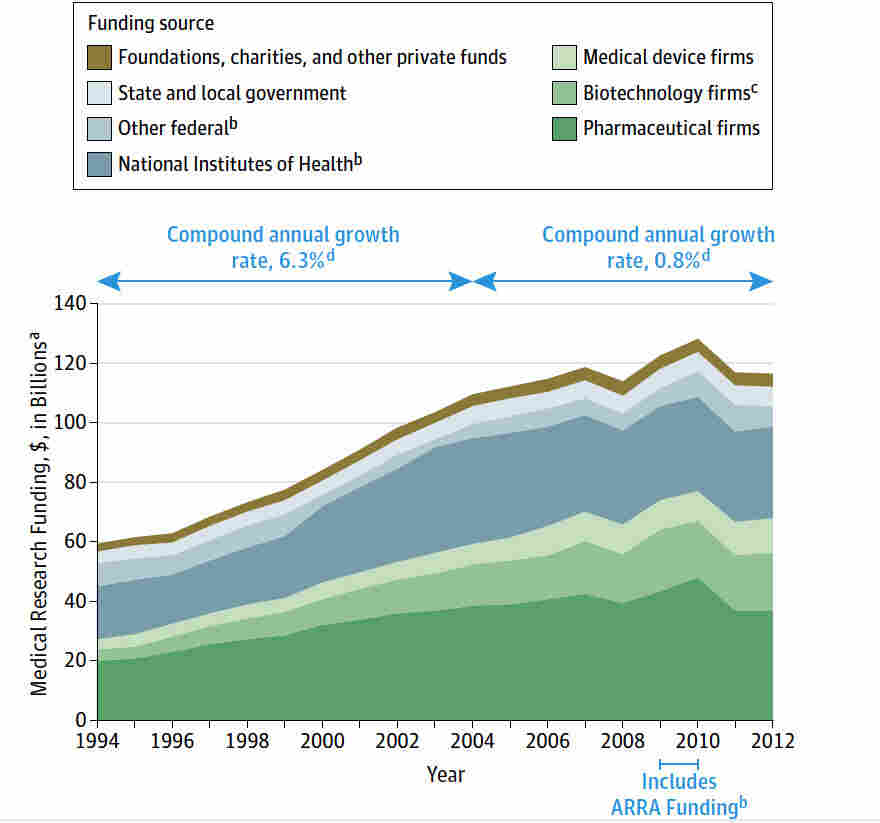
Medical research funding is crucial for advancing health innovations and ensuring patient safety in clinical trials. However, recent funding cuts have raised significant concerns within the research community, particularly in relation to National Institutes of Health (NIH) research grants. The lack of adequate financial resources hampers the operations of Institutional Review Boards (IRBs), which are essential for overseeing research protocols and safeguarding the welfare of human participants. Without sufficient funding, the oversight mechanisms that protect volunteers in studies could weaken, potentially leading to adverse effects on patient safety. The ramifications of these research funding cuts could jeopardize the positive outcomes that medical research, such as those conducted under Harvard’s guidance, aims to achieve.
The financial support for clinical studies, sometimes referred to as biomedical research backing or health investigation grants, plays a fundamental role in the advancement of medical science. As financial resources dwindle, the ability for research institutions to monitor and oversee studies effectively diminishes, raising serious concerns about ethical compliance and participant protection. Alternative funding channels are under scrutiny, particularly as federal research grants face cuts that could disrupt essential oversight functions provided by Institutional Review Boards (IRBs). The effects of this funding reduction ripple through the research community, affecting not just the researchers but also the volunteers who contribute to vital health advancements. The challenge is to maintain robust oversight and ethical standards in light of diminishing research dollars.
The Critical Role of Medical Research Funding in Patient Safety
Medical research funding is fundamental to advancing healthcare and ensuring patient safety. The National Institutes of Health (NIH) provides crucial grants that facilitate innovative studies, which include comprehensive assessments of patient welfare and safety. Without adequate funding, institutions like Harvard are unable to maintain compliance with institutional review boards (IRBs) that safeguard the rights of participants. The recent halt in funding has led to a disruption in this oversight, creating potential risks for patients involved in ongoing and new medical trials.
Moreover, research funding supports essential training programs for researchers and IRB members, enabling them to navigate the complexities of human subject research. This comprehensive funding structure ensures that ethical standards are maintained, minimizing risks while promoting more effective patient-centered outcomes. As federal funding shrinks, the integrity and efficiency of these processes come into question, ultimately affecting the safety measures in place for patients who volunteer for research.
Impact of Research Funding Cuts on Patient Trust
Cuts in research funding significantly impact public trust in medical research, particularly when past scandals have marred the history of such endeavors. Patients who participate in clinical trials rely on the belief that their safety is prioritized, but funding disruptions raise concerns about the thoroughness and ethical standards of IRB reviews. When studies are halted, as seen with Harvard’s SMART IRB, patient participation may decline as skepticism grows regarding the commitment of researchers to uphold safety regulations.
Restoring public confidence in research necessitates a clear demonstration of the value of funding for patient safety. Institutions must address the implications of funding cuts transparently and actively involve community members in discussions about the importance of ethical oversight. Only by doing so can the medical research community hope to rebuild trust, reassuring patients that their well-being is paramount to ongoing research efforts.
IRB Oversight: An Essential Safety Mechanism in Clinical Trials
The role of Institutional Review Boards (IRBs) in safeguarding patient safety cannot be overstated. These boards assess research proposals to ensure that the rights, welfare, and privacy of participants are protected throughout the study’s lifecycle. With the implementation of new NIH policies mandating single IRB review for multisite studies, the expectation for streamlined oversight becomes more critical than ever. Cuts to research funding inhibit these vital processes, jeopardizing the ethical oversight essential for participant safety.
Additionally, IRBs act as a check against potential harm, assessing risk versus benefit in research designs involving human subjects. An influx of funding allows for thorough review processes, training for IRB members, and robust engagement with researchers to instill a culture of safety and ethical responsibility. Without sufficient resources, the capability of IRBs to conduct rigorous evaluations diminishes, leaving patients vulnerable and the integrity of the research process at risk.
The Consequences of Research Funding Cuts on Collaboration
The current landscape of medical research is shaped not only by the innovative work of institutions but also by collaborative efforts across multiple sites. The SMART IRB model exemplifies how shared oversight can facilitate groundbreaking studies. However, recent funding cuts have hindered the ability to forge new collaborations, stalling progress on promising research areas, such as Alzheimer’s disease therapies. Researchers are finding themselves restricted by the bureaucracy brought on by a lack of financial support for essential infrastructure.
Moreover, as various institutions face funding shortages, the opportunity to innovate diminishes significantly. Each halted study not only affects the immediate research goals but also represents a setback in the potential benefits to patients. With rigorous collaboration being essential for comprehensive drug and treatment testing, ineffective funding can stifle advancements that are crucial for patient health outcomes.
Preserving Patient Rights Amidst Funding Challenges
The concept of informed consent is foundational to ethical research practices, ensuring that patients are fully aware of the implications of their participation. However, financial constraints threaten these practices as institutions divert their resources to mitigate the impacts of funding cuts. This can lead to rushed processes that compromise the clarity and honesty required in obtaining informed consent, potentially placing patients at risk.
Furthermore, when funding is limited, educational outreach to participants and communities suffers, making it difficult to engage and prepare prospective subjects adequately. Protecting the autonomy and rights of patients hinges on strong advocacy and support from funded research organizations, which are increasingly strained under the pressures of budget reductions. Addressing these concerns and re-establishing proper funding mechanisms will be essential in safeguarding patient rights in medical research.
Leveraging NIH Research Grants for Patient Protection
NIH research grants play a pivotal role in underpinning projects that prioritize patient protection and safety. These grants facilitate the establishment of comprehensive protocols for studies involving human subjects, ensuring that ethical standards are met, and risks are managed. Funding from the NIH is not merely financial support; it reflects a commitment to uphold the dignity and rights of individuals involved in medical research.
The recent reviews and adaptations in NIH policies, especially regarding IRB oversight, underscore the necessity for consistent funding. These regulations are designed to enhance patient safety by promoting rigorous review processes. Maintaining a steady stream of funding allows for continual adaptation and improvement of these safety protocols, fostering a more reliable research environment that prioritizes patient well-being.
Community Engagement in Medical Research Amidst Funding Cuts
Community involvement is essential in shaping the landscape of medical research, particularly in times of funding cuts. Engaging participants in the research process not only enhances transparency but also fosters a sense of trust and ownership over the research outcomes. Initiatives that place patients and communities at the forefront of research agendas are crucial for addressing their needs and concerns, especially when adverse funding decisions threaten to limit collaborative opportunities.
As academic and clinical research institutions work to navigate budget constraints, it is essential to maintain robust communication channels with community stakeholders. By listening to the voices of those impacted by research, including patient representatives, institutions can adapt their funding strategies to align with community needs, ultimately supporting better patient safety practices amidst challenging financial climates.
Historical Context and Its Implications for Modern Research
Historical injustices in medical research serve as a somber reminder of the ethical dilemmas that necessitate the safeguards we have today, including IRBs and stringent funding regulations. Events such as the Tuskegee syphilis study remain etched in public consciousness, driving home the significance of transparency and ethical oversight in medical research. Understanding this historical context is crucial for recognizing the importance of maintaining strong funding mechanisms that support ethical research practices.
The evolution of research ethics has led to robust structures designed to protect participants, but these frameworks require sustained investment to thrive. Funding cuts not only undermine current research efforts but can also open the door to past mistakes being repeated. Reinforcing the lessons learned from history will enable the medical community to adopt cautious, empathetic approaches that prioritize participant protection and trust, critical elements that underpin the success of future research.
Future Directions in Medical Research Funding and Patient Safety
Looking ahead, the medical research community faces the challenge of securing sustainable funding to ensure patient safety remains a fundamental priority. Innovative funding models that embrace public-private partnerships could emerge as a solution to the current limitations posed by federal cuts. By engaging diverse stakeholders, researchers can develop comprehensive strategies that encompass not just scientific inquiry but also community impact and safety measures.
Moreover, advocating for a reevaluation of funding priorities at national levels could lead to the reinstatement of essential financial support for research that prioritizes patient safety. Encouraging policymakers to recognize the long-term benefits of investing in research infrastructure will play a crucial role in shaping the future landscape of medical research, ultimately benefiting patients and communities alike.
Frequently Asked Questions
What impact do research funding cuts have on patient safety in medical research?
Research funding cuts significantly undermine efforts to ensure patient safety in medical research. For example, funding from organizations like the NIH is crucial for maintaining the Institutional Review Board (IRB) oversight, which protects the rights and welfare of human research participants. Without adequate funding, many studies face operational disruptions, halting recruitment and threatening the integrity of existing research efforts.
How does NIH research funding affect the oversight of medical studies?
NIH research funding is essential for the review and ongoing oversight of medical studies conducted on human participants. This funding supports the IRB processes that are legally required to ensure compliance with ethical standards. The suspension of NIH grants can consequently impede the oversight functions critical to safeguarding patient participants, which may lead to compromised research integrity.
What role does SMART IRB play in the context of medical research funding?
SMART IRB (Single Institutional Review Board) facilitates the ethical oversight of multi-site medical research funded by entities like NIH. It streamlines the IRB process, allowing for quicker approval of studies across multiple institutions. However, recent funding cuts disrupt this system, creating challenges in ensuring patient safety and delaying critical medical research initiatives.
Why are IRB reviews important in the landscape of medical research funding and patient safety?
IRB reviews are vital because they ensure that all aspects of medical research comply with ethical standards designed to protect patient safety. This oversight involves evaluating study designs, consent processes, and risk assessments. When research funding is cut, IRBs may struggle to operate effectively, which can result in inadequate protection for participants involved in medical studies.
How do federal grants like those from NIH influence the dynamics of collaboration in medical research?
Federal grants, such as those from NIH, are pivotal in promoting collaboration among research institutions. They fund initiatives like the SMART IRB, which simplifies multi-site studies. A halt in these grants can stifle collaborative efforts, leading to delays and complications in important medical research that relies on shared resources and expertise.
What historical context influences current practices in medical research funding and patient safety?
Historical events, such as the Tuskegee Syphilis Study, have profoundly shaped current practices in medical research funding and the emphasis on patient safety. These incidents underscored the necessity for robust ethical oversight and enforcement mechanisms, primarily provided by IRBs. Funding for these oversight functions ensures that lessons from the past continue to inform and improve the safety and rights of research participants today.
| Key Points |
|---|
| The Trump administration’s funding freeze of over $2 billion affects medical research and patient safety. |
| A stop-work order was issued for the SMART IRB contract, disrupting oversight of multi-site studies. |
| The SMART IRB facilitates collaborative oversight among hospitals, universities, and federal agencies. |
| IRBs ensure compliance with ethical standards in human research and protect participants’ rights. |
| NIH funds support necessary reviews, approvals, and oversight, which are crucial to participant safety. |
| Funding cuts can lead to halted research, increased harms to participants, and public skepticism towards medical studies. |
| Historical misdeeds in research highlight the importance of oversight and ethical conduct in studies today. |
| Continued funding and institutional support are vital for maintaining patient safety and advancing research. |
Summary
Medical research funding is critical for maintaining the safety and rights of patients involved in studies. The recent freeze in federal funding disrupts established oversight systems like SMART IRB, leading to concerns over the well-being of research participants. The implications of these funding cuts underscore the necessity of continued investment in medical research, particularly to uphold ethical standards and public trust.

Synaptic Plasticity: Groundbreaking Insights from Harvard Researchers
Synaptic plasticity is a fundamental process that underpins learning and memory formation, allowing our brains to adapt and reorganize in response to new information. Researchers at Harvard have recently developed an innovative technique designed to delve deeper into this complex phenomenon, providing invaluable insights for understanding neurological disorders such as dementia. By employing advanced brain mapping techniques, the team is now able to observe how synaptic connections strengthen and modify themselves during memory creation. This groundbreaking work, highlighted in Nature Neuroscience, emphasizes the critical role of synaptic architecture in forming memories and sheds light on potential therapeutic avenues for conditions that hinder cognitive function. As we uncover the intricacies of synaptic behavior, the implications for dementia research and enhancing learning capabilities become increasingly profound.
The study of synaptic dynamics often involves exploring concepts like synaptic modification or neuronal adaptability, which are essential for grasping how memories are formed and solidified in the brain. Terms such as synaptic strengthening and modulation are crucial as they represent the processes that allow for the flexibility necessary in our cognitive functions. Recent breakthroughs in brain mapping technologies have paved the way for delving into the molecular aspects of learning, potentially offering novel approaches to address issues related to various neurological conditions, including dementia. By utilizing the advanced Extracellular Protein Surface Labeling in Neurons (EPSILON) technique, scientists aim to unlock the underlying mechanisms that govern memory storage and retrieval. This revelation not only enriches our understanding of cognition but also guides future research towards effective interventions for memory-related impairments.
Understanding Synaptic Plasticity: The Foundation of Memory Formation
Synaptic plasticity is a key concept in neuroscience, referring to the brain’s ability to strengthen or weaken synapses based on activity levels. This dynamic process is essential for learning and memory formation, allowing us to adapt to new information and experiences. During memory formation, specific synapses undergo changes in response to stimuli, influencing our ability to recall information later. The groundbreaking technique developed by the Harvard researchers, known as EPSILON, provides a powerful tool to observe and analyze this intricate synaptic behavior at an unprecedented resolution, offering insights into the molecular mechanisms behind memory processes.
By focusing on proteins such as AMPARs, which play a crucial role in synaptic plasticity, researchers can map the intricate patterns that underlie memory formation. The ability to monitor these synaptic changes over time reveals how the brain encodes various memories, from simple facts to complex emotional experiences. This understanding is particularly vital in the field of dementia research, where synaptic dysfunction is often a hallmark of neurodegenerative diseases. Investigating synaptic alterations not only enhances our comprehension of memory but also paves the way for developing novel therapeutic interventions for neurological disorders.
Revolutionizing Dementia Research with Advanced Brain Mapping Techniques
Recent advances in brain mapping techniques, particularly through the application of the EPSILON method, are set to revolutionize dementia research. Traditional methods often fell short in capturing the real-time dynamics of synaptic interactions, which are critical for understanding how memory impairment occurs in conditions like Alzheimer’s disease. EPSILON offers a non-invasive way to visualize synaptic behavior with remarkable detail, enabling scientists to observe the rapid changes in synaptic strength associated with memory formation and recall.
As researchers apply EPSILON to study the mechanisms at play in dementia, they gain valuable insights into how synaptic plasticity is disrupted in affected individuals. This knowledge has profound implications for developing targeted treatments, as understanding the historical changes in synaptic architecture could inform strategies to restore or enhance cognitive function. With every breakthrough in brain mapping, the potential to mitigate the effects of neurological disorders continues to grow, inspiring hope for new therapeutic avenues that can significantly improve the quality of life for those affected by memory loss.
The Role of AMPARs in Memory and Learning Processes
AMPARs, or alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors, are pivotal players in the realm of learning and memory within the brain. These receptors facilitate synaptic transmission and are fundamental to the brain’s ability to modify its connections and strength during learning processes. The recent studies employing the EPSILON technique have illuminated the behavior of AMPARs, providing critical insights into their role in memory retention and retrieval.
Understanding the dynamics of AMPAR trafficking is essential for elucidating the mechanisms that govern memory formation. As highlighted in the research, there is a strong association between AMPAR activity and the expression of immediate early genes, which are indicators of neuronal activation during memory encoding. This linkage underscores the importance of AMPARs as both functional units of memory processing and targets for potential therapeutic strategies aimed at enhancing cognitive function or mitigating the cognitive declines associated with disorders like dementia.
Precision Techniques in Neuroscience: A New Era of Discovery
The introduction of precision techniques like EPSILON marks a significant advancement in neuroscience, opening new pathways for discovery in the study of learning and memory. This method allows researchers to delve deeper into the molecular underpinnings of synaptic plasticity, revealing the intricate details of how neurons communicate and form connections. By employing fluorescent labeling and high-resolution microscopy, scientists can track the movements and interactions of proteins critical for synaptic function, advancing our understanding of neural circuitry.
These groundbreaking techniques foster a new era of discovery that goes beyond surface-level observations, enabling the exploration of complex interactions within living brains. The potential to uncover the regulatory mechanisms of synaptic strength could inform broader research into neurological disorders, helping to identify biomarkers and therapeutic targets that could transform our approach to treating memory-related conditions.
Exploring the Connection Between Memory Formation and Neurological Disorders
Memory formation is intricately linked to various neurological disorders, making it imperative to understand the underlying biological mechanisms. Conditions such as Alzheimer’s disease and other forms of dementia disrupt the brain’s ability to create and retrieve memories, often stemming from deficits in synaptic plasticity. By exploring these connections, researchers aim to develop interventions that address the root causes of these disorders, rather than just managing symptoms.
Research leveraging techniques like EPSILON provides a clearer picture of how synaptic changes correlate with memory impairments. This integrative approach enhances our understanding of both memory formation and the dysfunction that leads to neurological disorders. Continued emphasis on elucidating these relationships will pave the way for innovative therapies designed to enhance memory function and ultimately improve patient outcomes.
The Future of Memory Research: Implications for Cognitive Health
As researchers continue to unlock the complexities of memory formation through innovative methodologies such as EPSILON, the implications for cognitive health are profound. With an enhanced understanding of synaptic plasticity and memory encoding, we are better positioned to develop targeted therapies that could preserve cognitive function throughout aging or recover it in individuals affected by neurodegenerative diseases. The potential for translating these research findings into clinical practice is rapidly becoming a reality.
The future of memory research not only holds promise for treating dementia but also for improving our general understanding of cognitive health across various populations. By supporting foundational research, scientists can facilitate the development of new technologies and interventions that promote brain health. This holistic approach, encompassing both basic and applied science, is essential for making strides towards preserving memory and enhancing learning capabilities throughout the human lifespan.
The Importance of Multi-Disciplinary Collaboration in Neuroscience Research
The advancement of neuroscience research, particularly in the fields of memory and synaptic plasticity, highlights the crucial role of multi-disciplinary collaboration. Teams comprising chemists, biologists, and neuroscientists—like those involved in the EPSILON study—can leverage their diverse expertise to gain a holistic understanding of complex processes. This cooperative effort fosters innovation, enabling the integration of various perspectives and techniques that yield more comprehensive insights into neurological functions.
By collaborating across disciplines, researchers can address the multifaceted nature of cognitive health and memory impairment. Such teamwork facilitates the flow of information and techniques, maximizing the potential for uncovering valuable discoveries that could lead to breakthrough therapies for conditions like dementia. The lessons learned from this collaborative spirit serve as a model for future research endeavors, emphasizing that the most significant advancements often arise from collective efforts.
Illuminating Historical Synaptic Plasticity: A New Perspective
The ability to illuminate historical synaptic plasticity represents a transformative leap in neuroscience research. By documenting the past history of synaptic changes in vivo, researchers can better understand how memories are formed and maintained over time. For instance, the EPSILON method allows scientists to observe the evolution of synaptic connections, offering insights into how specific experiences shape neuronal networks and, ultimately, memory.
This historical perspective on synaptic plasticity highlights the importance of timing and context in memory formation. Understanding when and how synapses are strengthened or weakened can reveal the foundational processes that underlie both healthy cognitive development and the decline observed in neurological disorders. Studies focused on this historical analysis will be crucial in developing effective interventions tailored to combat the effects of memory-related diseases.
The Path Forward: Innovations in Memory Therapeutics
As research progresses in the realm of memory formation and neurological disorders, the path forward lies in innovation and the application of newly discovered techniques such as EPSILON. These breakthroughs enable a more detailed mapping of synaptic interactions, paving the way for the development of effective memory therapeutics. By understanding the molecular basis of memory encoding and retrieval, researchers can identify specific therapeutic targets that could be manipulated to enhance cognitive function.
Future innovations may focus on harnessing the knowledge gained about synaptic plasticity to create medications, therapies, or interventions that restore synaptic communication and improve memory function. The ongoing collaboration between basic science and clinical applications is essential for realizing the full potential of these advancements. As we move forward, the goal should be to transform our discoveries into actionable strategies that support cognitive health and address memory impairments in populations affected by neurological disorders.
Frequently Asked Questions
What is synaptic plasticity and how does it relate to memory formation?
Synaptic plasticity refers to the brain’s ability to strengthen or weaken synapses, the connections between neurons, in response to increases or decreases in their activity. This process is crucial for memory formation, as it allows for the adaptation and reorganization of neural connections based on new experiences and information.
How does the new EPSILON technique advance our understanding of synaptic plasticity?
The EPSILON technique enables researchers to map the synaptic architecture associated with learning and memory at an unprecedented resolution. By focusing on proteins like AMPARs, which play a vital role in synaptic plasticity, this innovative method provides insights into how synapses strengthen or weaken during memory formation, offering potential breakthroughs in dementia research.
What role does synaptic plasticity play in neurological disorders like dementia?
Synaptic plasticity is essential for maintaining cognitive functions, and dysfunctions in this process are often linked to neurological disorders like dementia. Research into synaptic plasticity, particularly through techniques like EPSILON, may reveal underlying mechanisms of memory impairments seen in conditions such as Alzheimer’s disease.
Can brain mapping techniques contribute to our understanding of synaptic plasticity in learning?
Yes, advanced brain mapping techniques, such as EPSILON, enhance our understanding of synaptic plasticity by allowing researchers to visualize and analyze synaptic behavior in real-time. This increased precision helps elucidate the neural mechanisms behind learning and memory, thus aiding in the development of therapeutic strategies.
What are the potential implications of synaptic plasticity research for dementia therapies?
Research on synaptic plasticity, particularly using cutting-edge techniques like EPSILON, could lead to novel therapies for dementia. By improving our comprehension of synaptic changes during memory formation and their dysfunction in dementia, these studies may pave the way for targeted interventions to restore cognitive function.
| Key Point | Description |
|---|---|
| New Technique (EPSILON) | A method developed by Harvard researchers to map proteins essential for memory formation at a higher resolution. |
| Role of Synaptic Plasticity | Synaptic plasticity refers to the brain’s ability to strengthen or weaken synapses based on activity, crucial for learning and memory. |
| AMPAR Proteins | AMPARs (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors) are key proteins in synaptic transmission and plasticity. |
| Microscopy Method | Combination of fluorescent labeling and advanced microscopy enabled unprecedented observation of synaptic behavior. |
| Significance for Neurological Disorders | Insights from this technique could lead to new treatments for disorders like dementia and Alzheimer’s. |
| Research Implications | The ability to observe synaptic plasticity in real-time can enhance understanding of memory formation and its associated patterns. |
| Future Prospects | The technique could aid in exploring various cognitive processes and possibly lead to improved therapies for memory impairments. |
Summary
Synaptic plasticity is a fundamental process that allows the brain to adapt and reorganize in response to new information. Recent advancements, particularly the development of the EPSILON technique by Harvard researchers, have opened new avenues for understanding how memories are formed at the molecular level. This innovative method enables scientists to observe synaptic interactions in unprecedented detail, revealing the critical role of proteins like AMPARs in memory and learning. Such insights not only enhance our understanding of cognitive functions but also hold promise for developing therapies to treat neurological disorders, thereby addressing memory impairments that affect countless individuals.

Health Tracking: Revolutionizing Memory Formation Research
Health tracking has emerged as a vital tool in understanding the complex relationship between our cognitive functions and overall well-being. By closely monitoring physiological data, researchers can gain valuable insights into memory formation, the learning process, and the effects of synaptic plasticity on our brains. Recent neuroscience breakthroughs suggest that comprehensive health tracking could pave the way for innovative dementia treatment modalities. In fact, advanced techniques such as the newly developed EPSILON method are shedding light on the intricacies deep within our synaptic networks, offering hope for future therapies. By leveraging such knowledge, we move closer to unraveling the mysteries of how our brains adapt and respond to new information.
Exploring the realm of health monitoring not only encompasses tracking physical metrics, but also delves into cognitive health and its implications for neurological disorders. Terms such as wellness assessment and cognitive tracking collectively embody the practices that aim to enhance our understanding of memory and learning disruptions. By employing innovative methodologies, researchers can investigate the underlying mechanisms that dictate how memories are formed and retained. This shift in focus towards holistic health monitoring is increasingly recognized as essential for developing effective strategies to combat conditions like dementia. As scientists continue to unravel the brain’s complexities, the dialogue surrounding health tracking grows ever more vital in our quest for lasting cognitive health.
Understanding Memory Formation Through Synaptic Plasticity
Memory formation is a complex process intricately linked to synaptic plasticity, which refers to the brain’s ability to strengthen or weaken synaptic connections based on experience. This dynamism is founded on the molecular architecture of neurons, particularly the behavior of key proteins like AMPARs (alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors) that are critical for synaptic transmission. The study of synaptic plasticity not only sheds light on how we learn but also provides essential insights into various neurological disorders, including Alzheimer’s disease, where these fundamental processes are disrupted.
Research led by a team at Harvard has introduced groundbreaking techniques to map synaptic activity with unprecedented precision, allowing scientists to observe how these connections evolve during memory formation. This advancement emphasizes the importance of synaptic behavior in the learning process and reinforces the notion that understanding these mechanisms at a molecular level is crucial for developing effective treatments for memory-related disorders. The intricate interplay between synapses may reveal patterns that govern memory strength and longevity, potentially paving the way for new therapeutic interventions.
Revolutionizing Dementia Treatment with Neuroscience Breakthroughs
Recent breakthroughs in neuroscience, particularly concerning the mapping of synaptic plasticity, hold significant promise for advancing dementia treatment. As researchers decode the molecular underpinnings of learning and memory, they are uncovering potential therapeutic targets for neurodegenerative diseases. Techniques like EPSILON, which provide unparalleled insight into synaptic function, can help scientists better understand the mechanisms of dementia and other cognitive impairments, allowing for the development of targeted therapies that could restore or enhance memory function.
By identifying how synaptic connections change in response to learning experiences, researchers are better positioned to develop drugs or strategies that can either mimic these processes or enhance them in individuals suffering from memory loss. The hope is that by harnessing the intricate details of synaptic behavior, new treatment pathways can emerge, ultimately leading to improved quality of life for those affected by dementia and other similar conditions.
Health Tracking: Monitoring Synaptic Changes for Improved Cognitive Health
Health tracking has become a vital part of modern wellness strategies, and its application in neuroscience could signify a radical shift in how we understand cognitive health. By leveraging advancements in technology, such as those introduced by Harvard researchers, health tracking can now include monitoring synaptic changes associated with memory and learning. This could enable individuals to gain insights into their cognitive health and potentially identify early signs of neurodegenerative diseases.
As we explore the relationship between synaptic plasticity and cognitive function, tools that provide real-time tracking of synaptic behavior become invaluable. These health tracking methods, integrated with the latest neuroscience breakthroughs, could empower individuals to take proactive steps in maintaining their cognitive health. With early identification and intervention, the trajectory of disorders such as Alzheimer’s could significantly shift, opening up new avenues for treatment and disease management.
The Intersection of Fluorescent Labeling and Memory Research
Fluorescent labeling has emerged as a powerful tool in the realm of neuroscience, particularly in understanding memory formation and synaptic interactions. This technique, which allows researchers to visualize specific proteins and their behavior within neurons, has been instrumental in creating a clearer picture of synaptic plasticity and its role in learning processes. With innovations such as the EPSILON method, scientists can illuminate the intricate dynamics of synapses, revealing how memories are encoded at a molecular level.
The intersection of fluorescent labeling and memory research not only enhances our understanding of cognitive functions but also uncovers potential pathways for therapeutic advancements. By monitoring how synaptic connections are formed and modified, researchers are gaining insights that could lead to the development of effective interventions for cognitive impairments, marking a transformative step in addressing conditions like dementia.
Exploring the Role of Neurons in Memory and Learning
Neurons are the building blocks of the brain, intricately responsible for communication and processing information necessary for memory and learning. Each memory we form is rooted in the complex web of synaptic connections between these neurons, mediated by the principles of synaptic plasticity. Understanding how neurons interact and adapt during the learning process can unlock new strategies for enhancing cognitive performance and tackling neurological disorders.
As research unfolds, the spotlight is on how neurons can change and reorganize themselves in response to new experiences. Insights gained from studying synaptic behavior can inform the development of cognitive enhancement strategies, offering hope for improving memory retention and recall. This line of inquiry is vital, especially in the context of aging populations facing the threat of dementia, as it paves the way for innovative therapeutic solutions.
The Future of Memory Research and Cognitive Enhancement
The future of memory research is bright, with ongoing studies poised to deepen our understanding of cognitive enhancement through synaptic plasticity. As researchers continue to dissect the fundamental processes that govern memory formation, the potential to develop interventions that enhance learning and memory grows exponentially. Techniques that map synaptic behavior, such as EPSILON, are at the forefront of this exploration, revealing the intricate dance of proteins that underpin our cognitive lives.
Looking ahead, these advancements promise to not only foster new therapies for conditions like Alzheimer’s and other forms of dementia but also unlock strategies for cognitive enhancement in healthy individuals. The implications for education, therapy, and overall cognitive health are profound, suggesting a future where memory and learning can be actively improved through scientifically-informed methods.
Investigating the Molecular Basis of Learning Processes
At the heart of learning processes lies a rich tapestry of molecular interactions that govern how we acquire, process, and recall information. Recent research has spotlighted the role of synaptic plasticity in facilitating these experiences, revealing that the molecular changes during learning are pivotal for memory consolidation. Understanding these intricacies not just refines our knowledge of basic neuroscience, but can also uncover new therapeutic routes for learning disabilities and other cognitive disorders.
Indeed, the investigation into the molecular basis of learning is crucial for advancing educational strategies and treatments. By unraveling how synaptic connections are forged during learning, we can design interventions that bolster these processes, promote better educational methods, and enhance overall cognitive function. This research is not merely academic; it has real-world applications that could transform how we understand and foster learning across all age groups.
The Role of Cognitive Neuroscience in Understanding Memory
Cognitive neuroscience serves as a bridge between the biological mechanisms of the brain and the psychological processes involved in memory and learning. This interdisciplinary field integrates insights from neuroscience, psychology, and education to provide a comprehensive understanding of how memories are formed, stored, and retrieved. As we delve deeper into the workings of the brain, the insights gained are pivotal for addressing cognitive impairments and enhancing learning capabilities.
Recent advancements in cognitive neuroscience highlight the significance of synaptic changes and their connection to memory formation. Understanding these processes can lead to effective strategies for both educational enhancement and clinical interventions for disorders such as dementia. By leveraging the tools and findings of cognitive neuroscience, we can foster environments that support optimal learning and memory retention for individuals at all stages of life.
Neuroscience Breakthroughs as a Pathway to Enhanced Learning
Neuroscience breakthroughs have revolutionized our understanding of learning, particularly with regard to the molecular underpinnings of memory. Technologies that allow for the observation of synaptic changes have unlocked new avenues of inquiry, revealing how experiences shape our neural connections. Such revelations not only enrich the academic understanding of the learning process but also offer practical applications for enhancing educational practices and therapeutic interventions.
As we stand on the precipice of further discoveries in the field of neuroscience, there is great potential for applying these insights to refine teaching methodologies, improve cognitive training programs, and develop therapeutic strategies for memory-related disorders. By harnessing the power of neuroscience breakthroughs, we can cultivate environments that promote effective learning and cognitive resilience, ultimately leading to a society better equipped to face the challenges of memory loss and cognitive decline.
Frequently Asked Questions
How does health tracking relate to memory formation in the brain?
Health tracking tools can help monitor cognitive functions, including memory formation, by tracking lifestyle factors such as sleep, nutrition, and physical activity that impact brain health. Through consistent health tracking, individuals can identify patterns that may influence their ability to learn and form memories, potentially mitigating risks related to conditions like dementia.
What role does synaptic plasticity play in health tracking for cognitive health?
Synaptic plasticity is crucial for learning and memory. Health tracking applications can incorporate activities that enhance synaptic plasticity, such as cognitive exercises and mental challenges, allowing users to optimize their brain’s adaptive capabilities. This proactive monitoring of brain health can also help detect early signs of conditions like dementia.
Can health tracking technologies assist in dementia treatment?
Yes, innovative health tracking technologies that monitor cognitive behaviors and daily activities can provide valuable insights for dementia treatment. By understanding how lifestyle habits affect memory formation and synaptic health, healthcare professionals can design personalized interventions to help manage symptoms and improve quality of life.
How can neuroscience breakthroughs enhance health tracking systems?
Neuroscience breakthroughs, such as the development of techniques like EPSILON that map synaptic behavior, can inform health tracking systems by providing deeper insights into how learning and memory function. This knowledge can be integrated into digital health tools, offering users recommendations on activities that support cognitive resilience and memory retention.
What are the benefits of using health tracking for learning processes?
Using health tracking for learning processes can lead to improved understanding of personal learning habits, sleep patterns, and overall cognitive health. By correlating health data with learning outcomes, individuals can refine their study techniques and environments to boost memory formation and retention, leading to more effective learning experiences.
How does the study of memories contribute to health tracking advancements?
Research into memory formation and its underlying mechanisms enriches health tracking advancements by highlighting the importance of factors like synaptic plasticity. By integrating findings from memory studies, health tracking can evolve to emphasize practices that enhance cognitive function and mitigate risks associated with memory-related disorders.
| Key Points | Details |
|---|---|
| New Mapping Technique for Memories | Harvard researchers developed a novel technique to study how learning and memories are formed, particularly focusing on synaptic plasticity. |
| Technique Name: EPSILON | Extracellular Protein Surface Labeling in Neurons (EPSILON) maps proteins important for neuronal communication, specifically AMPARs. |
| Importance of Synaptic Plasticity | Synapses form the foundation of memory, and synaptic plasticity allows adaptation in response to new information. |
| Applications to Neurological Disorders | The insights from EPSILON may lead to new therapies for conditions such as Alzheimer’s and dementia. |
| Research Collaboration | The study involved a team of researchers, including students and postdoctoral scholars from Harvard and the Howard Hughes Medical Institute. |
| Future Implications | EPSILON will be distributed globally for further research on synaptic strength and cognitive functions. |
Summary
Health Tracking is becoming increasingly important as new research sheds light on the molecular mechanisms underlying learning and memory formation. The groundbreaking technique developed at Harvard, EPSILON, not only enhances our understanding of synaptic plasticity but also opens doors to potential treatments for neurological disorders like dementia. As research continues, effective health tracking methodologies can play a crucial role in monitoring cognitive health and developing therapeutic strategies that address memory impairments.
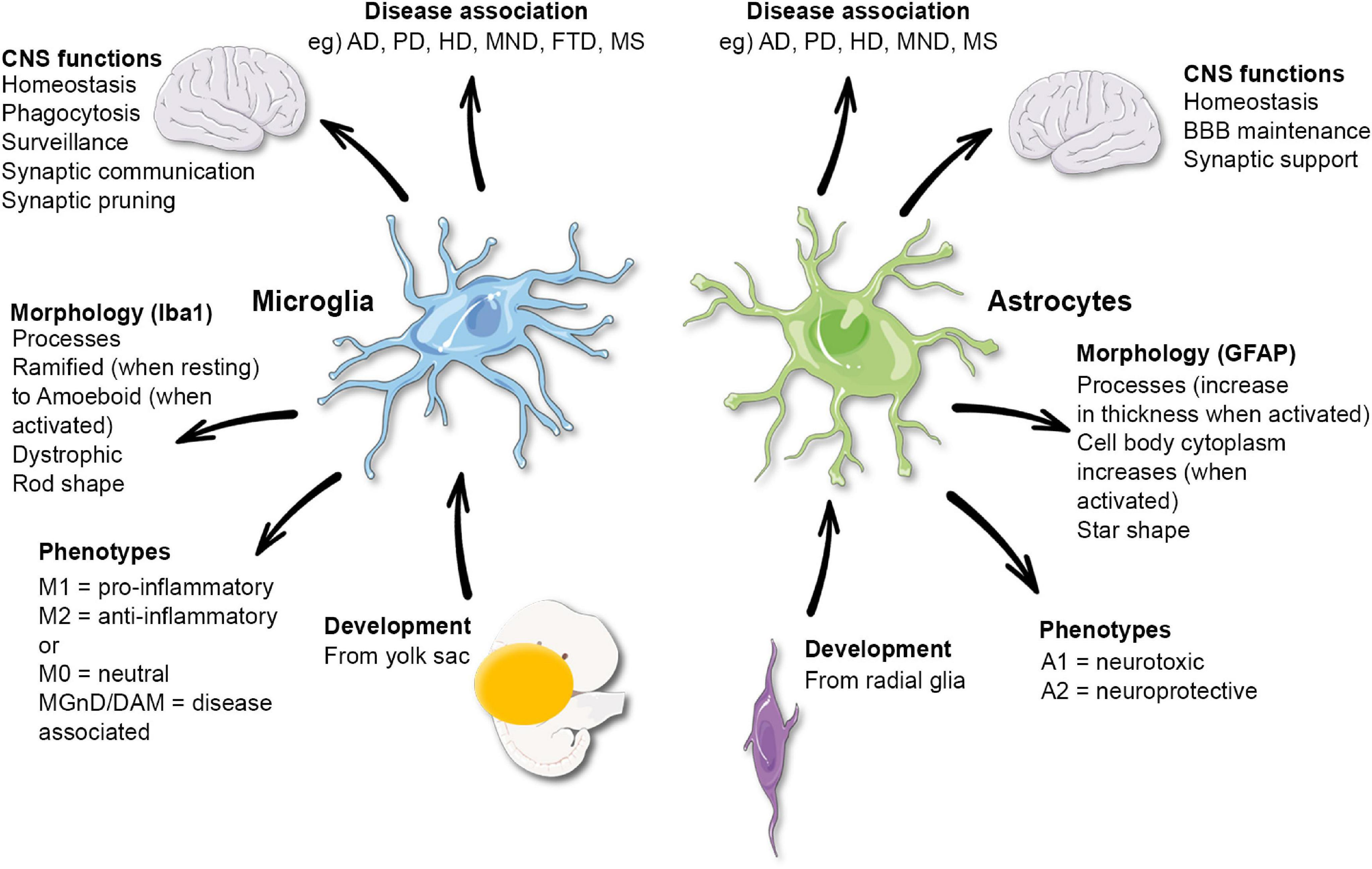
Microglial Research: A New Frontier in Alzheimer’s Treatment
Microglial research has become a pivotal area of study in understanding the complex interplay between the brain’s immune system and neurodegenerative diseases such as Alzheimer’s disease. These specialized cells are critical for maintaining brain health, as they monitor for signs of damage and engage in vital processes like synaptic pruning, the removal of unnecessary neuronal connections. However, recent findings indicate that dysregulated microglial activity may exacerbate conditions like Alzheimer’s, leading to detrimental outcomes. Pioneering work by researchers such as Beth Stevens has illuminated these cellular processes, offering hope for new biomarkers and treatment strategies for millions affected by cognitive decline. As science continues to uncover the roles of microglia in disease, we edge closer to innovative interventions that could transform patient care.
Research surrounding glial cells, particularly microglia, stands at the forefront of unraveling mysteries surrounding neurodegenerative disorders. These cells constitute the brain’s immune defense, helping to eliminate damaged neurons and engaging in synaptic remodeling, essential for healthy brain function. Nevertheless, imbalances in microglial activation have been linked to disorders like Alzheimer’s and Huntington’s disease, raising questions about their dual role in health and disease. Investigations led by experts like Beth Stevens are shedding light on these mechanisms, fostering the development of novel diagnostic and therapeutic approaches. By delving deeper into the brain’s supportive cell populations, we may uncover critical insights that facilitate better management of cognitive disorders.
Understanding Microglial Cells in Neurodegenerative Diseases
Microglial cells are essential components of the brain’s immune system. These specialized cells constantly survey the brain for pathogens and debris, thereby playing a crucial role in maintaining neuronal health. In recent studies, particularly through the work of Beth Stevens, it has been revealed that microglia not only defend against infections but also engage in synaptic pruning — a process that fine-tunes neuronal connections during brain development. This dual role highlights the significance of microglial research in understanding various neurodegenerative diseases.
However, malfunctioning microglia can negatively impact brain health. When these cells begin to prune synapses excessively, they may contribute to the development of conditions such as Alzheimer’s disease and Huntington’s disease. Stevens’ research has illuminated how improper synaptic pruning by microglia is a pivotal factor in these disorders, leading to the loss of neuronal connections and cognitive decline. Thus, advancing our knowledge about microglial functions and dysfunctions is vital in unraveling the complexities of neurodegenerative diseases.
The Role of Synaptic Pruning in Alzheimer’s Disease
Synaptic pruning is a natural process that refines synaptic connections, ensuring efficient communication between neurons. In healthy brains, this process is crucial for learning and memory. However, in the context of Alzheimer’s disease, abnormal synaptic pruning mediated by microglia has been linked to neural degeneration. Research led by Beth Stevens demonstrates that misregulated pruning can exacerbate Alzheimer’s symptoms, as it may lead to the selective elimination of pivotal neural connections necessary for cognitive function.
Beth Stevens’ investigations into the role of microglial cells in synaptic pruning have opened up new avenues for therapeutic strategies. By developing a better understanding of how microglia behave in disease states, scientists are beginning to identify potential biomarkers for early detection of Alzheimer’s disease and other neurodegenerative conditions. This could have a profound impact on timing and efficacy of interventions, ultimately improving the quality of life for millions of individuals afflicted by these diseases.
Research Breakthroughs: The Impact of Beth Stevens’ Work
Beth Stevens’ groundbreaking research has transformed our comprehension of the brain’s immune system, particularly focusing on microglial functions. Her work has provided clarity on how these cells protect the brain while also uncovering the dark side of their activity in the context of neurodegenerative diseases. Significant findings from her lab have revealed that a disruption in microglial function can lead to worsening conditions in patients with Alzheimer’s disease, illustrating the complex interplay between immunity and neurodegeneration.
With substantial support from NIH and other federal agencies, Stevens has pursued vital research that bridges basic science with clinical applications. This has fostered groundbreaking advancements in identifying new treatment pathways, such as targeting microglial activity to improve synaptic health in neurodegenerative diseases. Her contributions underscore the importance of funding basic research, which lays the foundation for future innovations in combating disorders like Alzheimer’s.
The Future of Neurodegenerative Disease Treatment
As research into microglial cells continues to unveil their crucial role in neurodegenerative diseases, the future of treatment looks promising. The identification of new biomarkers, as highlighted in Beth Stevens’ work, paves the way for more precise and earlier interventions for diseases like Alzheimer’s. This shift from reactive to proactive treatment approaches could drastically alter the prognosis for millions of patients by allowing for timely and targeted therapies.
Moreover, the integration of findings from studies on microglia and synaptic pruning holds potential for developing novel drug therapies aimed at modulating microglial activity. By fine-tuning the balance of immune response in the brain, scientists hope to mitigate neural damage and restore cognitive functions. This holistic approach to understanding and treating neurodegenerative diseases emphasizes the interconnectedness of immune processes and neuronal health, presenting new opportunities for enhancing patient care.
Exploring Neuroinflammation in Alzheimer’s Disease
Neuroinflammation is increasingly recognized as a central player in the progression of Alzheimer’s disease. Microglial cells are not only involved in synaptic pruning but also in the inflammatory response within the brain. When these cells respond to injury or neurodegeneration, they can either promote healing or contribute to chronic inflammation that exacerbates disease progression. Understanding the nuances of this response is crucial for developing effective interventions.
Beth Stevens’ research has provided valuable insights into how neuroinflammation can be managed therapeutically. By investigating the mechanisms that lead to dysfunctional microglial responses, her studies aim to uncover methods to harness the beneficial aspects of microglial activity while dampening the harmful inflammatory processes. This dual approach opens up possibilities for creating treatments that could slow the progression of Alzheimer’s disease and improve outcomes for those affected.
Impact of Federal Funding on Alzheimer’s Research
Federal funding, particularly from organizations like the NIH, plays a vital role in advancing Alzheimer’s research. Prominent researchers like Beth Stevens have repeatedly emphasized how critical funding has been to their groundbreaking studies. It allows for innovative research that not only furthers our understanding of diseases like Alzheimer’s but also catalyzes the development of new therapies and diagnostic tools.
The success of Stevens’ lab showcases the tangible outcomes of such investments. By supporting exploratory research into microglial biology and neurodegeneration, federal funding has facilitated pivotal discoveries that may lead to better strategies for managing Alzheimer’s disease. Continuous investment in this field is essential to sustain progress, enabling scientists to tackle the complex challenges posed by neurodegenerative diseases.
The Genetics of Alzheimer’s Disease and Microglial Research
Recent advances in genetic research have shed light on the hereditary aspects of Alzheimer’s disease. Studies have identified genes that are linked with increased risk for developing this debilitating condition, and many of these genes are implicated in the functioning of microglial cells. By understanding the genetics behind Alzheimer’s, research can better inform targeted therapies that address the underlying causes of disease.
Beth Stevens’ work intersects with genetic research by exploring how specific genetic variations can alter microglial behavior and contribute to disease mechanisms. This intersection of genetics and immunology presents exciting opportunities for the development of gene therapy approaches aimed at normalizing microglial function, ultimately reducing the risk or severity of Alzheimer’s symptoms. Future investigations are likely to deepen our understanding of how genetic predispositions can inform therapeutic strategies.
The Role of Basic Science in Medical Advancements
Basic science research provides the foundational knowledge that drives advancements in medicine. By exploring fundamental questions about biological processes, scientists like Beth Stevens have laid the groundwork for significant breakthroughs in understanding diseases such as Alzheimer’s. This type of research is often supported by federal funding, which is crucial for investigating complex interactions within the brain.
The insights gained from basic science extend beyond theoretical knowledge; they inform clinical approaches that can directly benefit patients. For instance, Stevens’ revelations about microglial function could lead to new diagnostic markers or treatment protocols for Alzheimer’s disease. This highlights how the synergy between basic research and clinical application is vital for transforming scientific discoveries into practical solutions for neurological disorders.
Collaborative Efforts in Alzheimer’s Disease Research
Collaboration among researchers is essential in the battle against Alzheimer’s disease and other neurodegenerative disorders. By pooling expertise from various fields, scientists can tackle the multifaceted challenges posed by these conditions more effectively. Initiatives that encourage interdisciplinary collaboration, such as those seen in Stevens’ research, foster innovative solutions that might not have emerged in isolated studies.
Beth Stevens’ partnerships with other researchers and institutions exemplify the power of collaboration. By engaging with geneticists, neurologists, and other specialists, her work on microglia and synaptic pruning has the potential to reach new heights. This collaborative approach not only enhances the depth of research but also accelerates the translation of findings into meaningful therapies for Alzheimer’s patients, illustrating how teamwork is crucial in advancing the field.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s disease research?
Microglial cells are vital components of the brain’s immune system and play a significant role in Alzheimer’s disease research. These cells are responsible for patrolling the brain for damage and removing dead cells, a process known as synaptic pruning. In the context of Alzheimer’s, improper microglial activity can lead to excessive pruning and contribute to the progression of the disease, as highlighted in the research led by Beth Stevens.
How does microglial research relate to neurodegenerative diseases?
Microglial research is crucial in understanding neurodegenerative diseases like Alzheimer’s and Huntington’s disease. These immune cells not only protect the brain by clearing damaged cells but also participate in synaptic pruning during development. Abnormal pruning carried out by microglia can exacerbate neurodegenerative conditions, making this research essential for developing potential treatments.
What are the implications of Beth Stevens’ research on microglia in Alzheimer’s disease?
Beth Stevens’ research on microglia reveals their dual role in protecting the brain and potentially exacerbating Alzheimer’s disease through improper synaptic pruning. Her findings have led to the identification of new biomarkers and therapeutic targets for neurodegenerative diseases, representing a pivotal advancement in Alzheimer’s disease research and treatment possibilities.
What insights does microglial research provide about the brain’s immune system?
Microglial research offers profound insights into the brain’s immune system by illustrating how these cells respond to injury and disease. These insights are critical for understanding how inflammation and immune responses may influence the development of neurodegenerative diseases such as Alzheimer’s, highlighting the importance of microglia in maintaining brain health.
How do microglial cells affect synaptic pruning during brain development?
Microglial cells play a key role in synaptic pruning, a natural process during brain development where excess synapses are eliminated to enhance neural efficiency. However, improper regulation of this pruning can lead to issues associated with Alzheimer’s disease and other neurodegenerative disorders, as demonstrated by the research from Beth Stevens that emphasizes the complexities of microglial function.
Why is foundational research important in the field of microglial studies?
Foundational research is crucial in microglial studies as it lays the groundwork for understanding complex brain functions and diseases. Beth Stevens emphasizes that such curiosity-driven investigations are essential for uncovering mechanisms that govern microglial behavior, which can ultimately inform the development of new strategies to combat Alzheimer’s disease and related disorders.
| Key Point | Details |
|---|---|
| Microglial Cells | Act as the brain’s immune system, removing damaged cells and pruning synapses. |
| Impact on Alzheimer’s Disease | Improper pruning by microglia can lead to neurodegenerative diseases like Alzheimer’s and Huntington’s. |
| Research Funding | Beth Stevens’ research has been significantly funded by NIH and other federal agencies. |
| Foundation of Basic Science | Curiosity-driven research has led to discoveries fundamental to understanding microglial functions. |
| Recognition | Stevens received a MacArthur grant for her significant contributions to understanding microglia. |
| Future Implications | Research has potential to develop new biomarkers and treatments for Alzheimer’s and other disorders. |
Summary
Microglial research is crucial in the understanding of neurodegenerative diseases such as Alzheimer’s, as it uncovers the roles and functions of these immune cells in the brain. Beth Stevens’ groundbreaking work demonstrates how the improper functioning of microglia affects brain health and contributes to disease progression. Her findings highlight the importance of continued support for basic science research, which can ultimately lead to innovative treatments and a better future for those affected by Alzheimer’s. This ongoing investigation not only enhances our understanding of the brain but also paves the way for advancements that could significantly improve patient care.

Vaping Cessation Pill: FDA-Approved for Quitting Vaping
The vaping cessation pill, varenicline, has emerged as a game changer for those desperate to quit vaping, especially among teens and young adults. A recent clinical trial revealed that this FDA-approved smoking cessation medication significantly boosts the success rates of quitting vaping, demonstrating effectiveness more than three times that of placebo treatments. As vaping continues to rise, particularly among adolescents, the need for robust nicotine addiction treatment alternatives is increasingly urgent. With approximately a quarter of young adults and a notable percentage of high schoolers engaging in vaping, varenicline presents a critical avenue for health professionals to support these individuals in overcoming their dependence. This breakthrough research not only highlights the safety of varenicline but also underscores its potential to curb the alarming trend of vaping among teens.
In addressing nicotine dependency, the varenicline medication offers a promising route for those looking to break free from their vaping habits. Widely known as a smoking cessation drug, this FDA-recognized pill not only aids in reducing nicotine cravings but also supports behavioral therapy efforts for younger users. Recent studies have demonstrated its remarkable efficacy in helping adolescents and young adults successfully quit vaping, revealing a significant advantage over standard counseling methods. The rising prevalence of e-cigarette usage among youths has necessitated effective intervention strategies, making treatments like varenicline essential in combating nicotine addiction. Thus, as the search for effective vaping cessation solutions continues, varenicline stands out in the fight to ensure healthier futures for young individuals grappling with nicotine.”}]} If you have any further requests or need adjustments, feel free to ask! Enjoy your day! Thank you! Happy coding! Take care! Cheers! Best! Thank you! Regards! Take care! Happy coding! Enjoy your day! Thank you! Cheers! Best! Regards! Best! Thank you! Regards! Take care! Cheers! Enjoy your day! Thank you! Thank you! Best! Cheers! Best! Thank you! Happy coding! Take care! Cheers! Best! Thank you! Enjoy your day! Thank you! Cheers! Best! Regards! Take care! Happy coding! Enjoy your day! Thank you! Cheers! Best! Regards! Thank you! Enjoy your day! Thank you! Thank you! Best! Have a great day! Regards! Enjoy! Thanks for using this tool! Best! Thank you! Take care! Regards! Thank you! Best! Enjoy your day! Take care! Cheers! Best! Thank you! Best! Thank you! Cheers! Thank you! Enjoy your day! Thank you! Regards! Thank you! Best! Take care! Happy coding! Regards! Thank you! Cheers! Thank you! Best! Enjoy your day! Take care! Happy coding! Enjoy your day! Thank you! Thank you! Best! Regards! Thank you for your feedback! Thank you for using this tool! Best! Thank you! Cheers! Best! Thank you! Cheers! Thank you! Take care! Regards! Thank you! Enjoy your day! Cheers! Best! Thank you! Regards! Thank you! Best! Enjoy your day! Take care! Cheers! Best! Thank you! Regards! Thank you! Enjoy your day! Take care! Happy coding! Thank you! Regards! Thank you! Best! Have a great day! Thank you! Take care! Cheers! Best! Thank you! Regards! Thank you! Best! Cheers! Thank you! Enjoy your day! Thank you! Regards! Thank you! Best! Have a great day! Regards! Regards! Thank you! Cheers! Thank you! Regards! Take care! Happy coding! Enjoy your day! Thank you! Best! Thank you! Cheers! Best! Thank you! Regards! Thank you! Enjoy your day! Thank you! Take care! Thank you! Best! Cheers! Thank you! Regards! Thank you! Cheers! Enjoy your day! Thank you! Regards! Thank you! Cheers! Best! Thank you! Enjoy your day! Thank you! Best! Cheers! Take care! Thank you! Regards! Thank you! Cheers! Enjoy your day! Thank you! Take care! Regards! Thank you! Enjoy your day! Thank you! Thank you! Thank you! Enjoy your day! Regards! Thank you! Cheers! Thank you! Best! Enjoy your day! Regards! Thank you! Cheers! Thank you! Regards! Thank you! Enjoy your day! Regards! Best! Thank you! Regards! Thank you! Enjoy your day! Thank you! Best! Cheers! Thank you! Regards! Thank you! Cheers! Have a great day! Thank you! Regards! Thank you! Enjoy this tool! Thank you! Best! Have a great day! Thank you! Enjoy your day! Thank you! Take care! Regards! Best! Thank you! Cheers! Best! Thank you! Enjoy your day! Take care! Thank you! Best! Thank you! Cheers! Enjoy your day! Thank you! Best! Regards! Thank you! Enjoy your day! Thank you! Best! Enjoy your day! Take care! Cheers! Thank you! Regards! Thank you! Best! Enjoy this tool! Thank you! Have a great day! Thank you! Best! Take care! Thank you! Cheers! Thank you! Enjoy your day! Thank you! Best! Enjoy your day! Take care! Happy coding! Thank you! Regards! Thank you! Best! Have a great day! Thank you! Enjoy! Thank you! Best! Thank you! Enjoy your day! Thank you! Regards! Thank you! Enjoy this tool! Thank you! Have a great day! Thank you! Enjoy the tool! Thank you! Best! Regards! Thank you! Take care! Best! Thank you! Enjoy your day! Cheers! Thank you! Best! Enjoy your day! Take care! Thank you! Best! Thank you! Regards! Cheer! Thank you! Regards! Thank you! Best! Have a great day! Thank you! Enjoy this tool! Thank you! Best! Have a great day! Thank you! Regards! Thank you! Thank you! Best! Have a great day! Thank you! Cheers! Thank you! Best! Enjoy this tool! Thank you! Take care! Best! Thank you! Take care!
The Growing Concern of Vaping Among Teens
Vaping has become immensely popular among teenagers, posing serious health risks. Statistics show that approximately a quarter of young adults aged 18 to 25 vaped in 2023, while around 8 percent of high school students reported the same in 2024. This trend is concerning given that vaping products are often seen as less harmful alternatives to traditional cigarettes, yet they still expose users to significant health threats including nicotine addiction. The ease of concealment and use in public spaces only exacerbates this problem, making it essential to understand the impact of vaping on this vulnerable population.
Research indicates that early exposure to nicotine can alter brain development and increase susceptibility to further substance abuse, including drugs like cocaine later in life. This calls for urgent action to address the rise of vaping among teens. With a dire need for effective interventions, studies exploring various treatment approaches are crucial. By focusing on tailored cessation strategies, such as the recent findings regarding varenicline, health professionals can better assist young people in successfully quitting vaping and ultimately reduce the health risks associated with nicotine consumption.
Varenicline: A Game Changer in Vaping Cessation
Varenicline, an FDA-approved smoking cessation pill, has shown remarkable efficacy in helping teens and young adults quit vaping. A recent clinical trial conducted by Mass General Brigham revealed that participants who received varenicline were over three times more successful in quitting compared to those who were only provided with behavioral counseling. This medication acts on the same neural pathways as nicotine, easing withdrawal symptoms and cravings while also reducing the pleasure derived from vaping.
These encouraging results highlight the potential of varenicline as a primary tool in nicotine addiction treatment for younger populations. With the age group of 16 to 25 being particularly vulnerable to nicotine addiction, the implementation of varenicline could revolutionize how we approach vaping cessation. Given that varenicline is easily accessible and tailored to fit the needs of younger individuals, this breakthrough in vaping cessation could pave the way for healthier futures among adolescents.
The Importance of Behavioral Support in Quitting Vaping
While medications like varenicline play a vital role in helping individuals quit vaping, combining these with behavioral support significantly enhances success rates. The recent study demonstrated that participants who received not only varenicline but also weekly behavioral counseling and access to a text support service experienced the highest quitting rates. This multi-pronged approach addresses both the physical and psychological facets of nicotine addiction, which is essential for sustained cessation.
Behavioral counseling provides individuals with strategies to cope with cravings and triggers while fostering a supportive environment. Programs like ‘This is Quitting’ offer real-time support, empowering teens and young adults on their journey to quit vaping. By integrating such resources with pharmacological options, health professionals can cultivate holistic treatment plans, ultimately increasing the chances of long-term success in quitting vaping.
Understanding Nicotine Addiction and Its Implications
Nicotine addiction is a complex condition that affects millions of individuals, particularly the youth. Vaping has emerged as a major gateway for nicotine use among teens, and understanding this addiction is crucial for developing effective cessation strategies. Nicotine not only alters the brain’s chemistry but also creates a powerful dependence that can make quitting exceedingly difficult without appropriate support and treatment.
The implications of nicotine addiction extend beyond physical health; they also encompass mental well-being and behavioral issues. As adolescents grapple with the social and psychological pressures associated with vaping, the need for comprehensive approaches to nicotine addiction treatment becomes paramount. This includes not only pharmacological interventions like varenicline but also educational outreach and preventive measures aimed at reducing the initiation of vaping among young people.
The Role of Educational Outreach in Preventing Vaping
Educational outreach plays a critical role in preventing the initiation of vaping among teens and young adults. By raising awareness about the risks associated with vaping, including its addictive properties and potential for long-term health consequences, we can better arm youths with the information they need to make informed choices. Schools, community organizations, and health professionals can collaborate to implement programs that educate adolescents about the dangers of nicotine and vaping.
Moreover, effective educational strategies should incorporate interactive methods to engage teens, such as workshops and social media campaigns. These programs can demystify the allure of vaping and convey relatable messages that resonate with young audiences. By fostering a culture of informed decision-making, we stand a better chance of curbing the rising trend of vaping among high schoolers and empowering young individuals to quit or avoid nicotine products altogether.
Exploring Future Research on Vaping Cessation
The promising results from studies on varenicline indicate a need for ongoing research into vaping cessation methods, particularly among younger populations. Future investigations may explore various therapeutic approaches, such as combining medications with different types of counseling or integrating digital health interventions. The evolving landscape of vaping necessitates research that adapts to the latest trends and user behaviors.
Additionally, there is a critical need to look for effective strategies for even younger users, including pre-teens who may be exposed to vaping. Understanding factors that contribute to addiction in this demographic can inform preventive measures and treatment protocols tailored to their developmental stage. Continued exploration in this field is essential to combat the public health crisis posed by vaping and protect future generations from the dangers of nicotine.
Safe Use of Varenicline in Young Adults
Safety is paramount when prescribing any medication, especially for younger individuals. Varenicline has shown not only effectiveness in aiding vaping cessation but also safety among the study participants. Reports indicated that none of the young adults who quit vaping transitioned to cigarette smoking, alleviating concerns about potential adverse outcomes often associated with nicotine withdrawal.
Healthcare providers must prioritize safety when considering treatment options for nicotine addiction. By recommending varenicline, alongside appropriate monitoring and support, young adults can be guided through addiction recovery without falling back into traditional smoking habits. Understanding the safety profile of varenicline reinforces its place as a viable option in public health efforts aimed at reducing nicotine dependence.
Integrating Supportive Services in Cessation Programs
Incorporating supportive services into cessation programs is essential for maximizing the success rates of those attempting to quit vaping. The study showcased the benefits of adding behavioral counseling and text-based support to pharmacological treatments such as varenicline. Such services not only augment the chances of quitting but also provide ongoing motivation and encouragement throughout the cessation journey.
Supportive services should be tailored to accommodate the unique needs of younger populations. This may include mobile applications that deliver personalized tips, counseling services via messaging, and resources that connect them to their peers who are also attempting to quit. By fostering a supportive network, individuals may feel more empowered to overcome their nicotine addiction and sustain their efforts in quitting vaping.
Addressing Vaping as a Public Health Priority
The rise of vaping, particularly among youth, has emerged as a significant public health crisis that needs immediate attention. Health professionals, educators, and policymakers must work collaboratively to prioritize strategies that reduce vaping rates and provide effective cessation resources. The recent findings regarding varenicline underscore the necessity of implementing FDA-approved treatments specifically catered to the younger demographic.
Efforts must extend beyond individual treatment plans to address systemic factors contributing to the vaping epidemic. This may involve regulatory measures to limit access to vaping products, implementing robust educational campaigns, and fostering community support systems. Conclusively, treating vaping cessation as a fundamental public health priority will help safeguard the future health of adolescents and young adults.
Frequently Asked Questions
What is the vaping cessation pill varenicline and how does it help quit vaping?
Varenicline is an FDA-approved smoking cessation pill that aids in quitting nicotine vaping. It works by targeting nicotine receptors in the brain, reducing withdrawal symptoms and cravings. In clinical trials, young adults who took varenicline were shown to have three times more success in quitting vaping than those receiving only behavioral counseling.
Can varenicline be prescribed to teens for vaping cessation?
Yes, varenicline can be prescribed to individuals aged 16 to 25 seeking to quit vaping. The recent studies indicate that this medication is effective and safe for younger populations struggling with nicotine addiction.
What are the success rates of using varenicline for quitting vaping among teens?
In a study involving participants aged 16 to 25, 51% of those taking varenicline successfully quit vaping after 12 weeks, compared to only 14% of those on placebo. This highlights the effectiveness of varenicline as a vaping cessation pill.
How does the FDA-approved smoking cessation pill varenicline differ from behavioral counseling for vaping cessation?
While behavioral counseling addresses the psychological aspects of nicotine addiction, varenicline, as an FDA-approved smoking cessation pill, provides a pharmacological approach that directly reduces cravings and withdrawal symptoms, enhancing overall success rates for quitting vaping.
What age group benefits most from the vaping cessation pill varenicline according to recent studies?
Recent studies indicate that teens and young adults aged 16 to 25 significantly benefit from varenicline when attempting to quit vaping, showing a higher success rate compared to placebo and behavioral therapy alone.
Is nicotine addiction treatment available for young adults who vape?
Yes, nicotine addiction treatment is available for young adults who vape, with varenicline being a prominent option. This pill is effective in treating nicotine dependence among individuals aged 16 to 25, helping them quit vaping.
What should I consider before starting varenicline for quitting vaping?
Before starting varenicline, it’s essential to consult with a healthcare provider who can assess your health history and suitability for this FDA-approved smoking cessation pill, ensuring it aligns with your quitting goals.
Are there any side effects associated with varenicline for vaping cessation?
While varenicline is generally considered safe for smoking cessation, like all medications, it can have side effects. It’s crucial to discuss these with a healthcare provider when considering this treatment for quitting vaping.
| Key Points |
|---|
| FDA-approved smoking cessation pill (varenicline) helps teens and young adults quit vaping effectively. |
| Clinical trials show varenicline users had three times the success rate of quitting vaping compared to the placebo group. |
| The study included 261 participants aged 16 to 25 and tracked success rates at 12-week and 24-week marks. |
| 51% of those taking varenicline quit vaping at the 12-week point compared to 14% in the placebo group. |
| This is the first study focused on vaping cessation in this vulnerable age group. |
| Varenicline can safely be prescribed to anyone aged 16-25 looking to quit nicotine vaping. |
| No participants who quit vaping turned to cigarettes, indicating safety of the treatment. |
Summary
The vaping cessation pill, varenicline, has proven to be an effective tool for young individuals looking to quit vaping. With its FDA approval and a successful clinical trial confirming a threefold increase in quitting rates among users, varenicline represents a promising option for adolescents facing nicotine addiction. This innovative approach not only aids in cessation but also demonstrates a commitment to addressing public health concerns associated with vaping among youth.

Global Youth Well-Being: Insights From a Major Study
Global youth well-being has emerged as a critical topic in recent discussions surrounding the health and happiness of younger generations worldwide. A significant study conducted by Harvard researchers highlights alarming trends regarding youth flourishing, particularly in wealthier nations, where financial well-being does not necessarily correlate with a fulfilling life. This groundbreaking “Global Happiness Study” reveals a concerning disconnect between economic status and overall mental health and youth satisfaction. Findings suggest that many young individuals face unique challenges that undermine their happiness and sense of purpose, raising questions about the effectiveness of current investments in their development. Understanding and addressing the multi-faceted nature of global youth well-being is now more essential than ever to foster environments conducive to thriving youth populations everywhere.
The welfare of young people around the world is increasingly recognized as a cornerstone of societal progress. Discussions about youth thriving often encompass various aspects, such as emotional resilience, financial stability, and meaningful connections within communities. Recent revelations from a global investigation into well-being underscore the stark contrasts in experiences among the youth, especially in nations boasting advanced economies. These insights shed light on the intricate relationship between mental health and youth development, challenging preconceived notions about happiness linked solely to wealth and material success. By exploring alternative metrics of fulfillment and connection, we can better support the next generation’s journey toward flourishing lives.
Understanding Global Youth Well-Being
Global youth well-being is a multifaceted concept that encompasses various aspects of health, happiness, financial security, and relationships among young people across different cultures. Recent studies highlight that while financial resources are often assumed to be a direct contributor to overall happiness, they may not be as significant as previously thought. For instance, the Global Flourishing Study reveals that middle-income countries actually rank higher in youth flourishing than wealthier ones, bringing to light the complexities surrounding the correlation between economic status and emotional well-being.
Factors such as strong familial relationships, community ties, and personal experiences during childhood play a critical role in shaping the overall well-being of youth. The research conducted by Harvard emphasizes the importance of investing in these relationships to enhance the quality of life among young people. Furthermore, the study calls into question the adequacy of current investments made in youth by various governments, particularly in wealthier nations where rising rates of mental health issues are observed among young adults.
The Connection Between Financial Well-Being and Youth Happiness
Interestingly, the Global Flourishing Study asserts that financial well-being does not automatically equate to higher levels of happiness among youth. In fact, the findings suggest that countries such as Indonesia, which struggle economically, exhibit surprisingly high levels of youth satisfaction due to strong social connections and supportive community environments. This challenges the conventional wisdom that emphasizes wealth accumulation as being paramount to achieving a flourishing life.
Moreover, the data reveals how youth in lower-income settings may cultivate resilience and strong social bonds that foster emotional support, leading to improved mental health outcomes. Such observations underline the necessity for policymakers to prioritize holistic development strategies that encompass social aspects alongside financial ones, enabling young individuals to thrive not just economically but also socially and emotionally.
Insights from the Global Happiness Study
The Global Happiness Study, which examines various indicators of well-being across multiple nations, emphasizes that mental health and youth flourishing significantly intersect with social determinants of happiness. This research aligns with findings from Harvard that indicate youth in communities with robust support systems report higher levels of satisfaction and emotional well-being, regardless of their financial status.
In light of these insights, it becomes essential to reassess how societies define success and happiness. Traditional metrics, which often focus on GDP and material wealth, should expand to include qualitative measures of flourishing—such as community engagement, emotional health, and personal fulfillment. Enhanced understanding of these dimensions will play a pivotal role in shaping effective interventions that nurture the holistic development of youth.
Mental Health Challenges Among Young People
Mental health continues to be a pressing concern for youth worldwide, with rising rates of anxiety and depression noted in many developed nations. The findings from Harvard’s research point to a significant gap in flourishing between younger and older adults, suggesting that current cultural and social pressures may disproportionately affect the mental health of the younger population. The study illustrates how these challenges manifest distinctly across various demographics and geographies.
Addressing youth mental health requires a comprehensive approach that considers the underlying factors contributing to distress, including social isolation, academic pressures, and familial dynamics. As emphasized by the researchers, fostering supportive environments through community engagement and developing initiatives aimed at strengthening familial relationships could yield substantial benefits for the mental health of young people.
Economic Development and Its Impact on Youth Flourishing
The comparative analysis of flourishing among nations sheds light on the paradox of economic development and youth well-being. While economically developed countries may have greater resources, this study reveals that richer nations may not be delivering optimal conditions for their young populations regarding happiness and mental health. For instance, Japan, despite its wealth, recorded the lowest levels of social connectivity and emotional satisfaction among youth.
Finding a balance between economic growth and enhancing the quality of life for youth is crucial. The research invites policymakers to prioritize social and emotional learning alongside traditional economic metrics. Such an approach could redefine how societies invest in their youth, ensuring that development strategies contribute positively to both financial security and emotional flourishing.
The Role of Relationships in Youth Well-Being
Relationships are a fundamental component of youth well-being, as underscore by studies linking positive family interactions and fulfilling friendships to higher measures of happiness and interest in life. The Global Flourishing Study highlights that regions where young people report strong social ties—whether with family or friends—tend to exhibit enhanced emotional health and resilience. This suggests that cultivating social environments could be a key strategy for improving youth outcomes.
Additionally, fostering connections among young people can mitigate the effects of mental health issues that are increasingly prevalent in today’s society. Programs aimed at improving interpersonal relationships and community involvement can serve as protective factors, leading to greater flourishing among the youth demographic. Thus, investing in activities that promote relationship-building is essential for enhancing overall youth well-being.
Policy Implications for Enhancing Youth Flourishing
Findings from Harvard’s Global Flourishing Study have significant implications for policies directed at youth development. The study encourages governments and organizations to invest more strategically in initiatives that address both the emotional and social needs of young people, rather than purely focusing on economic metrics. Such a shift could help foster an environment where youth can thrive holistically.
Moreover, embracing a multidisciplinary approach that recognizes the interconnectedness of financial well-being, mental health, and community engagement could help bridge the gap between youth needs and available resources. By aligning policies with research findings, we can work toward creating societies where youth not only survive but flourish, leading to a brighter future for all.
The Impact of Spiritual Well-Being on Youth Flourishing
Spiritual well-being, often overlooked in discussions about youth flourishing, emerges as a critical component in the Global Flourishing Study. Research indicates that regular engagement in spiritual practices, whether through organized religion or personal belief systems, correlates with improved mental health and happier youth. Spirituality can provide a sense of purpose and belonging that mitigates feelings of isolation and despair among young people.
The study suggests that programs encouraging spiritual exploration—without imposing specific beliefs—could enhance well-being among youth. While the approach may vary across cultures, fostering spiritual connections can provide resilience and a sense of community, essential for holistic youth flourishing. Such initiatives could significantly enrich the emotional landscape that young individuals navigate in their formative years.
Lessons from the Global Flourishing Study for Future Generations
As researchers continue to dissect the results of the Global Flourishing Study, their findings present numerous lessons for future generations. One key takeaway is the necessity for a comprehensive understanding of youth well-being that transcends financial metrics. The acknowledgment that social, emotional, and spiritual dimensions are equally, if not more, important to youth well-being serves as a powerful reminder for structure policies that support diverse developmental needs.
Furthermore, ongoing analysis of this longitudinal study will likely reveal essential patterns in how various factors influence youth flourishing over time. By focusing on these insights, communities and policymakers can adapt strategies that not only prioritize immediate needs but also anticipate future challenges, creating sustainable paths for youth well-being across the globe.
Frequently Asked Questions
What is the impact of financial well-being on global youth well-being?
Financial well-being plays a significant role in global youth well-being, but recent studies, including the Global Flourishing Study, indicate that financial status alone does not guarantee a flourishing life for youth. Countries with lower economic status, like Indonesia, have higher rankings in youth flourishing compared to wealthier nations, highlighting the complex interplay between financial security and overall well-being.
How does mental health influence youth flourishing globally?
Mental health is a crucial aspect of global youth well-being. The Global Flourishing Study emphasizes that good mental health leads to higher levels of flourishing among youth. Factors such as strong familial relationships, community support, and access to mental health resources significantly contribute to the mental well-being of young people, influencing their overall happiness and life satisfaction.
What does the global happiness study reveal about youth flourishing trends?
The global happiness study, particularly the findings of the Global Flourishing Study, reveals troubling trends in youth flourishing, with many young individuals experiencing a decline in well-being during their late teens and twenties. This shift from the traditional U-shaped life satisfaction pattern suggests that youth today face more challenges than earlier generations, emphasizing the need for increased investment in their well-being.
What did the Harvard research find regarding relationships and youth flourishing?
Harvard research, particularly through the Global Flourishing Study, found that positive relationships with parents and peers are universally linked to higher levels of youth flourishing. Youth who reported strong, supportive relationships tend to exhibit better mental health, greater life satisfaction, and increased resilience, which are essential for achieving overall well-being.
How can societies enhance global youth well-being?
To enhance global youth well-being, societies need to focus on holistic approaches that include financial support, mental health resources, and the cultivation of meaningful relationships. The findings from studies like the Global Flourishing Study suggest that improving community support systems and prioritizing youth engagement can significantly contribute to their overall flourishing and happiness.
Why does the Global Flourishing Study question the association between wealth and youth well-being?
The Global Flourishing Study questions the association between wealth and youth well-being by revealing that financial prosperity does not always correlate with higher flourishing levels among youth. Countries such as Indonesia ranked higher than wealthier nations in terms of youth well-being, suggesting that social connections, community life, and personal relationships may be more critical factors influencing youth flourishing than mere economic wealth.
| Key Points | Details |
|---|---|
| Study Findings | A major global study indicates a significant lack of well-being among youth, particularly in wealthy nations, challenging the notion that financial status ensures flourishing. |
| Youth Well-Being Trends | The traditional U-shaped curve of flourishing is shifting towards a J-shape, indicating lesser satisfaction among young adults in their late teens to twenties. |
| Study Demographics | The Global Flourishing Study involved 203,000 participants across 22 countries, incorporating various demographics to assess well-being. |
| National Rankings | Indonesia ranked highest in well-being despite lower economic status, while the U.S. was 15th in a ranking excluding financial indicators. |
| Factors Influencing Flourishing | Strong family relationships and frequent religious participation were consistently linked to higher levels of adult flourishing. |
Summary
Global youth well-being is increasingly recognized as a significant concern, especially in affluent nations where the study indicates that financial resources do not guarantee fulfillment or satisfaction. This research compels us to re-evaluate our investment in youth, focusing not only on economic growth but also on fostering meaningful relationships and environments conducive to flourishing. It emphasizes the need for a holistic approach to development that prioritizes emotional and social well-being alongside financial success.

Global Health: Atul Gawande’s Appeal for Action
Global health is at a critical juncture, as highlighted by Atul Gawande, a prominent voice in the health community and former leader at USAID. The recent global health crisis has exposed serious vulnerabilities in our health and science infrastructure, particularly after the drastic cuts to USAID that have dismantled its vast network of programs. This decline in global health leadership not only jeopardizes the wellbeing of millions worldwide but also shifts the landscape of international health initiatives toward uncertainty. The impact of USAID cuts has been profound, stalling critical public health advancements and threatening scientific progress that has historically saved lives. In an era where collaboration and robust science infrastructure are more crucial than ever, Gawande’s call to action urges us to recommit to the enduring pursuit of global health.
The state of worldwide healthcare faces unprecedented challenges, as articulated by Gawande, who emphasizes the urgent need for strategic involvement in international health initiatives. The dismantling of vital programs has led to a significant setback in medical advancements, highlighting the importance of effective leadership and sustainable science frameworks. As nations navigate the repercussions of these actions, the role of collaborative health efforts becomes even more paramount. Understanding the nuances of this situation is key to rallying support and fostering innovation in disease prevention and treatment. With a recommitment to global health, we can ensure that essential healthcare services remain accessible for underserved populations across the globe.
The Impact of USAID Cuts on Global Health
The recent cuts to the U.S. Agency for International Development (USAID) have led to a significant setback in the realm of global health. With over 85% of its programs terminated and staff laid off, millions worldwide are facing dire consequences. Atul Gawande, former head of USAID’s Bureau for Global Health, emphasizes that these changes have not only diminished the agency’s capacity to respond to outbreaks but also undermined critical public health interventions that saved countless lives. For instance, USAID’s initiatives significantly reduced the emergency response time for diseases like Ebola and flu, a rapid response crucial in managing public health crises.
Moreover, the cessation of funding has jeopardized essential health programs that target maternal and child mortality rates. Gawande notes that preventive measures alone reached approximately 93 million women and children, adding vital years to their lives. This illustrates that the impact of USAID cuts will be felt for years to come as nations grapple with increased mortality and health inequities. Continuing to support and rebuild global health infrastructure is paramount, as the long-term ramifications of inaction could exacerbate existing public health crises.
Restoring Global Health Leadership
As the world grapples with the consequences of reduced funding and support for global health initiatives, restoring leadership in this arena is critical for the U.S. Gawande argues that while USAID cannot simply revert to its previous operational state, there remains an opportunity to innovate and develop a sustainable framework for global health. This restoration hinges on a renewed commitment to building partnerships with universities, medical centers, and international bodies to revive the essential programs and collaborative efforts that have historically kept global health threats at bay.
Furthermore, strong global health leadership must engage in proactive strategies that address the fundamental challenges facing health systems worldwide. By leveraging advancements in science and medicine, the U.S. can lead in creating effective health policies and interventions that significantly improve health outcomes. This call to action for renewed global collaboration relies on developing robust science infrastructure that is resilient to political changes, ensuring that critical health services and research continue uninterrupted, thus safeguarding the health of vulnerable populations across the globe.
The Role of Science Infrastructure in Public Health
The strength of any nation’s public health system lies in its science infrastructure, which acts as the foundation for innovative health solutions and research advancement. As Gawande points out, the Trump administration’s disinvestment in agencies like USAID has severely weakened the science infrastructure necessary for effective health responses. This critical component not only involves funding but also fostering relationships with scientific communities to cultivate research and findings that address pressing health challenges. A strong science infrastructure ensures the swift transfer of knowledge and resources, which is crucial during health emergencies when time is of the essence.
Investing in science infrastructure also promotes diversity in health research, leading to comprehensive solutions that are culturally and contextually relevant to diverse populations. Ensuring that researchers across different demographics can contribute to health discussions leads to better outcomes in program design and implementation. Additionally, refocusing attention on this vital area encourages young scientists and healthcare professionals to join the public health workforce, reinforcing the commitment to tackling future health challenges with innovative and informed approaches.
Encouragement Amidst Challenges in Global Health
Despite the daunting challenges posed by reduced funding and support, Atul Gawande remains committed to encouraging future generations to stay resilient in the field of global health. He advises students and emerging health professionals to recognize the critical role they will play in addressing global health disparities. The ongoing attack on health infrastructures may cast shadows of uncertainty, but the need for knowledgeable and passionate individuals in this field is increasingly vital. Gawande’s own journey reflects the resilience required to navigate such hurdles, inspiring others to pursue innovation and collaboration in their careers.
Additionally, the call for maintaining focus on global health initiatives serves as a rallying point for advocacy and activism among health professionals and communities. Gawande urges that regardless of the governmental landscape, the expertise of healthcare workers is indispensable in overcoming public health crises. He emphasizes that the collective effort in science, medicine, and advocacy can lead to transformative change, ultimately empowering individuals to reclaim their roles as leaders in global health.
The Future of Global Health Initiatives
Looking forward, the future of global health initiatives hinges on a collective commitment to rebuilding and enhancing the mechanisms that address health crises. Gawande encourages stakeholders to pivot towards innovative methodologies that not only restore previous capabilities but also build a foundation for future advancements. The transformation of USAID’s governance could present an opportunity to implement insights garnered from past challenges, ultimately leading to a more adaptable and forward-thinking approach to global health.
Moreover, sustainable solutions for global health require an emphasis on multi-sector collaboration, bringing together public health officials, researchers, and policymakers to address health disparities. These collaborations can lead to the creation of comprehensive and responsive health systems that are better equipped to handle crises. By fostering such partnerships, nations can develop robust frameworks that prioritize health equity and leverage scientific advancements for the greater good, ensuring a healthier future for all.
Mobilizing Resources for Global Health
The mobilization of resources is a fundamental aspect of fostering strong global health programs. As highlighted by Gawande, without adequate funding and support systems, initiatives that historically saved lives will be severely hampered. Mobilizing financial and human resources not only strengthens the operational capacity of organizations like USAID but also enables the implementation of groundbreaking health interventions. As nations face increasing health burdens, it is imperative to develop strategies that effectively allocate resources towards preventative and responsive health measures.
In addition to traditional funding avenues, resource mobilization can leverage private sector investments and philanthropy to ignite innovation in health solutions. The collaborative efforts of governments, corporate partnerships, and non-profit organizations can create a holistic approach to public health that encompasses preventive care, education, and infrastructure development. Ensuring that resources are effectively and equitably distributed must remain a priority, as this ultimately shapes the quality of health services accessible to vulnerable populations.
Technical Assistance in Global Health
Technical assistance is essential to enhancing the capacity of countries to improve their health systems effectively. Gawande articulates that the strength of organizations like USAID lies not only in their funding but also in their expertise and guidance in executing health programs. Technical assistance involves providing the necessary tools, training, and support to implement health interventions successfully, which can elevate nations’ capabilities to address public health issues. Through collaboration with global health organizations, countries can adopt best practices and scalable solutions tailored to local contexts.
Furthermore, investing in technical assistance enables countries to elevate their health metrics significantly. Gawande emphasizes that the incremental improvements achieved through concerted efforts, like increasing vaccination rates from 60% to 90%, illustrate the importance of persistent, hands-on support. By fostering a collaborative environment where knowledge and expertise can flow freely, technical assistance becomes a powerful catalyst for developing resilient health systems capable of withstanding future crises.
Engaging Youth in Global Health Discourses
Engaging youth in global health discourses is crucial for driving innovative solutions that tackle emerging health challenges. Gawande’s address to students and faculty emphasizes that their fresh perspectives and expertise can foster transformative practices within public health. By encouraging a diverse range of voices in dialogues surrounding global health, transformative ideas can arise that potentially reshape existing paradigms and strategies, ultimately creating a more equitable healthcare landscape.
Challenges facing public health are multifaceted, and the involvement of young leaders is paramount in navigating these complexities. Initiatives aimed at empowering youth in global health education and advocacy can energize movements for change, enabling them to not only participate in discussions but also be champions for impactful health initiatives. As the next generation of health professionals rises, their engagement becomes not just beneficial but essential for the evolution of public health on a global scale.
The Importance of Community Health Initiatives
Community health initiatives play a pivotal role in enhancing public health outcomes at the local level. Gawande acknowledges that leveraging community resources can bridge the gap in healthcare access, particularly for marginalized populations. These grassroots movements foster trust and facilitate preventive care measures that are integral for reducing disease prevalence. By investing in community health, societies can build sustainable systems that empower individuals to take charge of their health and well-being.
Moreover, local community initiatives can serve as a model for larger health systems, showcasing effective frameworks that prioritize prevention and health promotion. Engaging communities in health program design ensures that interventions are contextually appropriate and culturally sensitive. This localized approach reinforces the notion that while global health demands collaboration, the actual transformation occurs when individuals are empowered to enact change within their own environments.
Frequently Asked Questions
What is the impact of USAID cuts on global health efforts?
The cuts to USAID have had a devastating effect on global health efforts, significantly reducing the funding and support necessary for programs that monitor and respond to health crises. With more than 85% of its programs terminated, millions of people are left without essential healthcare services, jeopardizing advances made in areas such as maternal and child health, infectious disease response, and overall health infrastructure.
How does the global health crisis affect research at institutions like Harvard?
The global health crisis exacerbated by the halt of USAID funding has put immense pressure on research initiatives at institutions such as Harvard. Programs aimed at tackling significant health challenges—like those at Ariadne Labs and the National Institutes of Health—face funding freezes, severely impacting ongoing research and collaboration that are critical for public health advancement.
What role does global health leadership play in responding to health emergencies?
Global health leadership is crucial in coordinating responses to health emergencies. Despite recent challenges, effective leaders can help mobilize resources and implement strategies that enhance medical responses to outbreaks, as demonstrated by USAID’s ability to reduce disease response times significantly when fully funded.
How has Atul Gawande influenced global health initiatives during his tenure at USAID?
Atul Gawande’s leadership at USAID was pivotal in advancing global health initiatives, particularly in improving health outcomes for women and children. His efforts in establishing rapid response systems for outbreaks and enhancing maternal health services optimized the delivery of healthcare across multiple countries, even leading to a six-year increase in life expectancy for many.
What are the long-term consequences of the global health void left by cuts to USAID?
The long-term consequences of the cuts to USAID include deteriorating health infrastructure in recipient countries, increased vulnerability to diseases, and setbacks in progress made in combating epidemics. This could lead to a resurgence in preventable diseases and ultimately hinder global health advancements that have been achieved over decades.
Can the global health community recover from the disruptions caused by funding cuts?
While the disruptions have been extensive, recovery is possible through renewed investment in global health and science infrastructure. As leaders in academia and health emerge to fill the gaps left by diminished USAID efforts, a sustained commitment to global health initiatives is vital for restoring and improving health outcomes worldwide.
How does science infrastructure contribute to effective global health strategies?
A robust science infrastructure is fundamental to effective global health strategies as it supports research, enables timely health data collection, and facilitates the development of innovative medical solutions. This infrastructure is essential for addressing public health challenges and implementing evidence-based practices that can reduce disease incidence and improve overall health outcomes.
| Key Point | Details |
|---|---|
| Gawande’s Experience | Atul Gawande served as head of USAID’s Bureau for Global Health, focusing on health infrastructure and talent. |
| Impact of USAID Cuts | Dismantling of USAID led to significant loss of staff and programs, harming global health initiatives. |
| Emergency Response | USAID reduced emergency response time for global outbreaks from over two weeks to under 48 hours. |
| Maternal and Child Health | Programs helped save 93 million women and children, adding six years to life expectancy. |
| Future of Global Health | Gawande expressed hope but uncertainty about the future U.S. role in global health leadership. |
| Call to Action | Gawande emphasized the importance of expertise and commitment in global health efforts. |
Summary
Global health is at a critical juncture, influenced profoundly by the recent structural changes at USAID. Atul Gawande highlights the severe consequences of budget cuts and staff reductions, which have jeopardized essential health initiatives worldwide. Despite these challenges, Gawande remains optimistic about the future of global health, urging continued commitment from future leaders and experts in the field. He emphasizes that the work of global health remains vital, as it directly affects the well-being of millions, and calls for action to support and protect these essential programs.
Bile Imbalance: A Major Link to Liver Cancer Uncovered
Bile imbalance is increasingly recognized as a crucial factor in the development of liver diseases, especially hepatocellular carcinoma (HCC), the most prevalent form of liver cancer. This imbalance arises from the dysregulation of bile acids, which are essential for fat digestion and metabolic regulation. Recent studies have uncovered how an abnormality in bile production can lead to liver injury, inflammation, and ultimately, liver cancer. The FXR receptor plays a significant role in maintaining bile acid homeostasis, and its dysfunction can exacerbate these conditions. Understanding the connection between bile imbalance and liver disease not only opens new avenues for treatment but also emphasizes the importance of maintaining gut health in preventing severe outcomes like liver cancer.
Liver dysfunction can manifest through various conditions, often highlighted by the disruption of bile production and regulation. This phenomenon, frequently described as disturbances in biliary function, presents a significant risk factor for various liver ailments. When bile acids, which serve both digestive and hormonal functions, fail to regulate properly, it can trigger a cascade of health issues that may culminate in serious conditions like hepatocellular carcinoma. The involvement of specific molecular players, like the FXR nuclear receptor, is critical for maintaining balance, indicating the intricate relationship between bile acids, liver health, and disease progression. Recognizing these connections is essential for developing targeted therapies and prevention strategies in the fight against liver-related illnesses.
Understanding Bile Imbalance and Its Consequences
Bile imbalance, a key factor in various liver diseases, occurs when the production and regulation of bile acids go awry. As bile acids are crucial for fat digestion and absorption, any disruption can lead to severe consequences for liver health. For instance, excessive bile acids can cause liver injury, setting the stage for more serious conditions such as hepatocellular carcinoma. This imbalance has been linked to a host of other metabolic disorders, highlighting the liver’s central role in regulating overall bodily functions.
Recent studies have shed light on the mechanisms behind bile imbalance, revealing its intricate relationship with liver disease and cancer. The liver’s ability to produce bile is tightly controlled; any interference with this process can lead to an accumulation of bile acids in the liver, resulting in inflammation and fibrosis. This cycle is particularly concerning as it may predispose individuals to hepatocellular carcinoma, the most prevalent form of liver cancer, emphasizing the need for targeted therapies that can restore bile acid homeostasis.
The Role of FXR in Bile Acid Regulation
The Farnesoid X receptor (FXR) plays a pivotal role in the regulation of bile acids, acting as a crucial sensor that maintains bile acid levels within a healthy range. When FXR function is compromised, typically through the inhibition by YAP—an important protein implicated in cell growth and cancer—bile acids can accumulate excessively, leading to detrimental effects on liver function and increased cancer risk. Understanding the role of FXR in bile acid metabolism has opened new avenues for treatment options aimed at restoring normal liver function.
Recent research has demonstrated that enhancing FXR activity could mitigate the adverse effects of bile acid accumulation. By promoting the excretion of bile acids and correcting the imbalance, it may be possible to prevent the progression of liver damage and reduce the risk of developing hepatocellular carcinoma. Targeting FXR pharmacologically presents a promising strategy for developing new treatments for individuals suffering from liver diseases related to bile imbalances.
Linking Bile Acid Metabolism to Liver Disease
The metabolism of bile acids is integral to liver health; disturbances in this process can lead to a cascade of health issues, including liver disease and cancer. Bile acids not only assist in digestion but also play crucial roles in signaling pathways that regulate metabolism, inflammation, and immune responses. When bile acids are not properly metabolized, the consequences can be severe, leading to increased risk for conditions like hepatitis and hepatocellular carcinoma. Research into these metabolic pathways is vital for understanding how to protect liver health.
Research has shown that interventions aimed at correcting bile acid metabolism may improve outcomes for patients already facing liver disease. For example, treatments that enhance bile acid transport or promote FXR activation can decrease liver inflammation and fibrosis, ultimately lowering the risk of hepatocellular carcinoma. Recognizing the links between bile acid dysregulation and liver disease is crucial for developing preventative strategies and treatment protocols.
The Importance of Early Detection in Liver Cancer
Early detection of liver cancer, particularly hepatocellular carcinoma, significantly influences treatment outcomes and survival rates. With bile imbalance being a precursor to liver cancer, recognizing the signs of liver dysfunction can lead to timely interventions. Many liver diseases, characterized by bile acid irregularities, may present subtle symptoms that can easily be overlooked, making patient education and routine screening crucial components in the fight against liver cancer.
Emerging protocols that include monitoring bile acid levels could serve as an additional tool in the early detection of liver cancer. By correlating bile acid dysregulation with increased cancer risk, healthcare providers can implement preventive measures sooner, ultimately aiming to improve patient prognosis. Continued research into the relationship between bile metabolism and liver cancer is vital for developing comprehensive screening strategies.
Potential Therapies Targeting Bile Acid Secretion
As the understanding of bile acid metabolism and its role in liver disease progresses, so too does the exploration of potential therapies aimed at enhancing bile acid secretion. Treatments designed to stimulate bile flow or correct metabolic disruptions may hold the key to preventing liver complications, including hepatocellular carcinoma. Such therapies could aim to enhance FXR function or support the body’s natural bile acid transport mechanisms, representing a novel approach toward liver health.
In experimental studies, interventions that successfully increase the expression of bile acid transport proteins or inhibit their reabsorption have shown promise in reducing liver injury associated with bile imbalance. These therapeutic strategies are particularly exciting as they could not only alleviate symptoms but also block the pathways leading to liver cancer development, providing a well-rounded approach to managing liver diseases.
The Connection Between Liver Disease and Metabolic Disorders
Liver disease is often interconnected with various metabolic disorders, many of which can be traced back to disruptions in bile acid metabolism. Conditions such as obesity and diabetes have been linked to alterations in bile acid profiles, which can lead to liver inflammation and an increased risk of hepatocellular carcinoma. This intersectionality underscores the importance of taking a holistic view when addressing liver health and metabolism, focusing not just on the liver alone but considering the wider implications of systemic health.
Understanding this complex relationship opens the door for multidimensional treatment strategies that address both liver health and metabolic disorders. By integrating lifestyle modifications, dietary interventions, and targeted therapies aimed at restoring bile acid balance, healthcare providers can create comprehensive treatment plans for patients at risk of liver disease and metabolic complications.
Research Advancements in Bile Metabolism
Ongoing research into bile metabolism has unveiled critical insights that may lead to transformative therapies for liver disease. With key findings highlighting the role of molecular switches like YAP and FXR, scientists are better equipped to understand how to manipulate these pathways for therapeutic benefit. This research not only furthers our knowledge of liver biology but also paves the way for innovative treatment options for conditions like hepatocellular carcinoma.
Additionally, the exploration of bile acids as potential signaling molecules opens new vistas for understanding liver homeostasis and its disruption in disease. By continuing to delve into the molecular underpinnings of bile metabolism, researchers may identify novel intervention points that can restore balance and promote liver health, ultimately reducing the incidence of liver cancer and improving patient outcomes.
Lifestyle Factors Affecting Bile Production
Lifestyle choices significantly influence bile production and regulation, directly impacting liver health. Diet, physical activity, and even psychological stress can alter bile acid homeostasis, leading to imbalances that predispose individuals to liver disease. For instance, diets high in saturated fats can disrupt bile acid synthesis, resulting in overproduction or insufficient bile, both of which may contribute to liver complications and increase the risk of developing hepatocellular carcinoma.
Adopting a balanced diet rich in fiber and low in unhealthy fats, combined with regular exercise, can help maintain healthy bile production and support liver function. Moreover, managing stress through mindfulness practices can further bolster liver health, making lifestyle modifications a pivotal aspect of preventing bile imbalance and reducing the likelihood of liver disease.
Future Directions in Liver Cancer Research
As the scientific community continues to unravel the complexities of liver cancer, future research will likely focus on identifying biomarkers related to bile acid metabolism that could predict liver disease progression. Exploration of new pharmacological agents that stimulate FXR and modulate bile acid levels will be central to developing targeted therapies aimed at treating and preventing hepatocellular carcinoma.
Collaborative efforts among researchers, clinicians, and healthcare institutions will be essential in translating these discoveries into clinical practice. By prioritizing research into the interplay between bile metabolism, liver function, and cancer development, we can forge a path toward better management strategies and improve outcomes for patients suffering from liver disease and cancer.
Frequently Asked Questions
What is bile imbalance and how is it related to liver cancer?
Bile imbalance refers to the disruption in the production and regulation of bile acids by the liver, which can lead to liver diseases, notably hepatocellular carcinoma (HCC). Research indicates that this imbalance may trigger inflammation and fibrosis in the liver, escalating the risk of developing liver cancer.
How do bile acids affect liver health and contribute to liver disease?
Bile acids play a crucial role in digestion and metabolic regulation. An imbalance in bile acids can cause liver injury and contribute to diseases such as liver cirrhosis and hepatocellular carcinoma. Dysregulation leads to toxic accumulation of bile acids in the liver, resulting in specific liver diseases.
What role does the FXR receptor play in bile acid metabolism and liver disease?
The FXR (Farnesoid X receptor) is vital for maintaining bile acid homeostasis. When bile acid levels are imbalanced, FXR function can be inhibited, resulting in the overproduction of bile acids that can damage liver cells and promote the development of liver diseases such as hepatocellular carcinoma.
How can addressing bile imbalance potentially aid in liver cancer treatment?
Addressing bile imbalance can provide promising avenues for liver cancer treatment. Enhancing FXR function or promoting bile acid excretion may help restore homeostasis, reduce liver inflammation, and inhibit the progression to hepatocellular carcinoma.
What mechanisms lead to bile acid overproduction that is linked to liver cancer?
Bile acid overproduction linked to liver cancer occurs when molecular switches, like YAP, interfere with regulated bile acid metabolism. This disruption can lead to an accumulation of bile acids in the liver, causing cellular damage, inflammation, and increasing the risk of hepatocellular carcinoma.
Can lifestyle choices influence bile imbalance and liver disease risk?
Yes, lifestyle choices such as diet, alcohol consumption, and physical activity significantly influence bile metabolism. Poor dietary habits and excess weight can exacerbate bile imbalance, increasing the risk of liver diseases, including hepatocellular carcinoma.
What are the potential therapeutic strategies to correct bile imbalance?
Potential therapeutic strategies include pharmacological stimulation of the FXR receptor, enhancing bile acid export proteins, and inhibiting the repressor functions of YAP. These interventions might restore bile acid homeostasis, reduce liver damage, and slow or prevent the progression of liver cancer.
| Key Points |
|---|
| Bile imbalances can lead to liver diseases, including liver cancer (HCC). |
| A crucial molecular switch regulating bile acids has been identified, offering potential treatment avenues. |
| Bile aids in fat digestion and also functions in metabolic regulation, showcasing its complex role in health. |
| YAP, a key protein, inhibits FXR, leading to bile acid overproduction and liver damage. |
| Activating FXR or enhancing bile acid excretion can block the negative effects of bile imbalance. |
| Research findings may lead to pharmacological solutions targeting FXR to combat liver cancer. |
Summary
Bile imbalance is a critical factor in liver health, significantly linked to the progression of liver cancer. Recent findings highlight the importance of regulating bile acid production to prevent liver damage and inflammation that can lead to hepatocellular carcinoma. Understanding the role of molecular switches in this process opens up new treatment possibilities, underscoring the need for further research in this area.
CRISPR Ethics: Balancing the Promise and Peril
CRISPR ethics is a burgeoning field of discussion that grapples with the ramifications of revolutionary CRISPR technology in gene editing. As scientists unlock the potential to modify genes associated with diseases like sickle cell disease, ethical concerns arise, prompting society to question the morality of such genetic modification. The promise of health equity through accessible treatments must be weighed against the risks of unintended consequences and the implications for human diversity. Is it our responsibility to alter the very fabric of our genetic makeup, or does the pursuit of cures overstep ethical boundaries? Understanding the delicate balance between innovation and moral considerations is crucial in this age of advanced gene editing ethics.
The ethical considerations surrounding CRISPR technology and gene editing extend far beyond mere scientific capabilities. With the advent of advanced genetic modification techniques, questions about the implications of altering human DNA emerge, especially as we confront conditions like sickle cell anemia. The debate centers on who should dictate the terms of genetic alterations, reflecting deeper societal values and beliefs about health equity. As we explore the potential to eradicate hereditary diseases, we must also assess the potential risks that come with such groundbreaking advancements. Ultimately, the discourse on gene editing ethics demands a nuanced understanding of both the science involved and the diverse perspectives on what it means to be human.
Exploring the Ethical Landscape of CRISPR Technology
The advent of CRISPR technology presents a monumental opportunity in the field of genetic modification, especially for treating debilitating diseases like sickle cell anemia. Yet, this power comes with complex ethical questions that challenge our understanding of humanity and the extent to which we should intervene in our genetic makeup. Science and ethics intersect profoundly when we consider whether it is right to alter genes, particularly for conditions deemed compatible with life. The debate revolves around who gets to decide which traits should be modified and what implications such decisions hold for individual autonomy and societal norms.
As we navigate the ethical landscape of gene editing, it becomes increasingly vital to consider the broader context of health equity. While CRISPR offers the potential for groundbreaking treatments, access to these innovations remains uneven. The high costs associated with genetic therapies raise concerns about who can afford to benefit from such medical advancements. As noted in discussions around CRISPR, the disparity in healthcare access necessitates a careful evaluation of both ethical practices and the potential reinforcement of existing inequalities within our health systems.
Health Equity: The Uneven Playing Field of Gene Editing
Health equity is a recurring theme in discussions surrounding CRISPR and gene editing technologies. As advancements promise cures for diseases like sickle cell, those who can access these innovations are often limited to wealthier populations, leaving marginalized communities at a disadvantage. This imbalance raises serious ethical questions about fairness. For instance, how do we ensure that breakthroughs in genetic modification do not exacerbate health disparities? It’s crucial to advocate for policies that promote equitable access to groundbreaking treatments, fostering a health system that serves all individuals, regardless of their socioeconomic status.
Moreover, the risks associated with gene editing technology necessitate a thorough investigation into the ethical ramifications of such innovations. If only a select few can afford the treatments, we might witness a widening gap in health outcomes, further entrenching societal inequalities. The key to ethical gene editing lies in inclusivity—developing healthcare solutions that prioritize the needs of various populations. As we explore the future of CRISPR, we must address these disparities head-on, ensuring that advancements in medical science lead to greater health equity rather than reinforcing existing hierarchies.
The Responsibility of Gene Editing: Making Difficult Choices
The responsibility surrounding gene editing is a crucial aspect of the ongoing conversation about the future of CRISPR. As highlighted by experts, the ability to edit genes offers the potential to eliminate diseases, but it also invites a host of moral dilemmas. For example, if parents could choose to enhance or modify traits of their unborn children, such as eliminating genetic predispositions to certain diseases or making aesthetic alterations, should they have the right to do so? These questions compel us to consider the implications of parental choice and the societal pressures that may accompany such capabilities.
Within this framework, we also have to contemplate the concept of ‘normalcy’ and the societal values that influence our definitions of what constitutes a ‘desirable’ trait. As emphasized by various speakers in recent discussions, individuals with disabilities like deafness argue that their conditions should be viewed as human variations rather than pathologies needing correction. This perspective challenges the ethical justification of gene editing for enhancement purposes and underscores the need for a nuanced conversation about the implications of such technology on human diversity.
The Unintended Consequences of Genetic Modification
While CRISPR technology holds the promise of reversing genetic disorders, it also comes with the potential for unintended consequences. The complexity of the genome means that altering one gene can lead to unforeseen effects on other traits and biological pathways. For instance, as mentioned in recent talks, editing genes controlling cholesterol might inadvertently affect other critical health functions, revealing the intricate web of genetic interactions that could complicate our understanding of health outcomes. This reality underscores the need for caution and thorough research before widespread application of gene editing technologies.
Understanding the ecosystem of genes is essential. The long-term outcomes of gene editing are uncertain, leaving us with the responsibility to evaluate not only the benefits but also the risks involved. As the scientific community advances in its capabilities, it is imperative to establish stringent guidelines and regulatory frameworks to ensure ethical practices. By doing so, we can protect against the potential for harmful repercussions while also embracing the incredible advances that CRISPR technology makes possible.
Ethical Governance of Gene Editing: Regulation and Oversight
The need for robust ethical governance surrounding gene editing is more pressing than ever as CRISPR technology becomes increasingly accessible. Discussions about regulation and oversight focus on preventing misuse and ensuring that genetic modifications are conducted safely and ethically. Experts argue that while some forms of gene editing are currently prohibited, such as germline editing, enforcement of these regulations can be challenging in a global context where practices may differ widely. This creates a scenario where ethical standards must be delineated and implemented across borders to prevent unethical experimentation.
Implementing effective regulatory measures requires international collaboration and dialogue among scientists, ethicists, policymakers, and the public. As the field evolves, it is crucial to engage various stakeholders in conversations about ethical oversight. This collective effort can help establish a consensus on best practices in gene editing while addressing the diverse ethical implications tied to this technology. Balancing innovation with ethical responsibility will be vital in shaping the future landscape of genetic modification.
Rethinking Genetic Modification: Cultural Perspectives and Human Variation
Cultural perceptions of gene editing significantly influence the dialogue surrounding CRISPR technology. Variations in beliefs about human diversity, disability, and what constitutes a ‘normal’ human condition play a critical role in shaping public opinion on genetic modification. For example, advocacy from communities with disabilities highlights the importance of recognizing human variation as a natural part of our existence rather than a condition that requires fixing. This calls for a broader understanding of the implications of genetic modifications and raises valuable questions about the societal norms we impose regarding health and wellness.
As we engage in discussions of genetic modification, it’s essential to include diverse cultural narratives and perspectives. By doing so, we can foster a more inclusive dialogue about what it means to be human and how CRISPR technology might redefine these concepts. Acknowledging the array of cultural contexts allows for a more comprehensive understanding of the ethical challenges posed by gene editing and encourages a dialogue that respects and values human differences.
The Future of CRISPR: Opportunities and Challenges Ahead
The future of CRISPR technology is poised at a crossroads of opportunity and ethical challenge. As researchers continue to uncover its potential, the excitement of curing previously untreatable conditions is tempered by important considerations about the implications of genetic modifications. The prospect of eradicating genetic diseases such as sickle cell anemia is incredibly promising; however, the accompanying ethical discourse plays a crucial role in guiding the technology’s application. Establishing a thoughtful approach to CRISPR’s future will be vital in harnessing its capabilities responsibly.
Looking ahead, the scientific community faces the challenge of balancing innovation with ethical considerations. How do we ensure that advancements in CRISPR lead to improvements in public health while preventing potential abuses of power or unintended consequences? By addressing questions of equity, governance, and cultural perspectives, researchers, policymakers, and the public can work together to shape a future where gene editing is directed toward the benefit of all, fostering a more just and equitable health landscape.
Innovations in CRISPR: Bridging Research and Real-World Applications
The ongoing innovations in CRISPR technology are not only exciting from a scientific standpoint but also hold transformative potential for real-world applications in medicine and healthcare. As efforts focus on translating lab discoveries into therapeutic solutions, the implications for conditions like sickle cell disease become increasingly tangible. However, this transition from bench to bedside brings forth ethical questions about the appropriateness and accessibility of these treatments.
To successfully bridge the gap between research advancements and practical applications, stakeholders must consider the ethical ramifications of deploying CRISPR technology. This includes addressing concerns surrounding informed consent, equitable access, and the long-term safety of gene-editing treatments. By fostering collaboration between researchers, ethicists, and healthcare providers, we can create a framework that promotes responsible innovation while ensuring that the benefits of CRISPR technology are accessible to all.
Public Perception of CRISPR and Genetic Editing Technologies
Public perception plays a significant role in shaping the future of CRISPR and genetic editing technologies. As these technologies become more prevalent, understanding how people feel about their ethical implications is crucial. Misinformation and fears surrounding gene editing can hinder progress and public support, making it essential to engage in transparent and informative dialogues. Educating the public about the possibilities and limitations of CRISPR will help demystify the technology and promote a more nuanced understanding of its ethical considerations.
Moreover, active engagement with diverse communities can help align scientific advancement with societal values. By listening to the concerns and aspirations of various populations, researchers and ethicists can better address public fears and work collaboratively toward a common goal. This approach not only enhances trust in scientific endeavors but also ensures that public desires and ethical standards are taken into account as CRISPR continues to evolve.
Frequently Asked Questions
What are the ethical concerns surrounding CRISPR technology?
CRISPR technology raises multiple ethical concerns, particularly regarding gene editing ethics. Key issues include the potential for genetic modification to exacerbate health inequality, as costly treatments may only be accessible to affluent individuals. Additionally, ethical dilemmas arise from altering germline cells, which could have long-lasting impacts not only on the individual but also on future generations. The decision of whether certain traits should be modified, especially in conditions like Down syndrome, is heavily debated, questioning who has the right to make such choices.
How does CRISPR impact health equity in treating conditions like sickle cell disease?
While CRISPR shows promise in curing conditions like sickle cell disease, its high cost (approximately $2.2 million per treatment) poses significant health equity challenges. Access to gene editing technology may be limited for lower-income populations, exacerbating existing health disparities. The ethical implications of who can afford these treatments and how they affect global health equity remain pressing questions in discussions about CRISPR technology.
Should parents have the right to use CRISPR for non-life-threatening genetic conditions?
The ethics of using CRISPR for genetic modification, particularly in cases of non-life-threatening conditions, are highly controversial. Many argue that it is not the parents’ right to decide on traits such as hearing ability in children born to deaf parents. This raises fundamental questions about identity, diversity, and the societal implications of ‘choosing’ characteristics, which lead to discussions about the nature of human variation.
What role does oversight play in the ethical use of CRISPR technology?
Oversight is crucial in ensuring the responsible application of CRISPR technology. While laws exist against cloning and germline editing, enforcement can be inconsistent, especially in countries with differing regulations like Russia and China. Ethical oversight is essential to prevent misuse of CRISPR, such as creating genetically modified soldiers or altering genes without considering long-term ramifications, highlighting the need for global standards in gene editing ethics.
Are there unintended consequences associated with CRISPR gene editing?
Yes, CRISPR gene editing can lead to unintended consequences, as the interactions within genetic sequences can be complex. For example, a modification intended to lower LDL cholesterol might impact other metabolic pathways, affecting insulin regulation and leading to unknown health issues. Understanding that genes are intricate and evolve over millions of years necessitates caution in applying CRISPR technology, emphasizing the ethical responsibility of scientists to consider potential repercussions.
| Key Points | Details |
|---|---|
| Introduction to CRISPR Ethics | N. Baer discussed ethical implications of gene editing. |
| Potential to Cure | CRISPR can cure diseases like sickle cell anemia but raises ethical questions. |
| Somatic vs. Germline Editing | Editing somatic cells can help individuals; germline editing affects future generations. |
| Ethical Decision Making | Who decides which conditions can be treated? Cost and health equity are major issues. |
| Cultural Perspectives | Should parents determine desirable traits for their children? |
| Oversight and Regulation | Concerns about illegal experimentation in countries with less oversight. |
| Unintended Consequences | Gene editing may have unforeseen effects on other biological functions. |
Summary
CRISPR ethics is a complex and critical discourse that centers on the moral implications of gene editing technology. While CRISPR offers groundbreaking opportunities to cure genetic diseases, it also raises profound ethical questions regarding the nature of human differences, the decision-making authority for gene editing, and the ramifications of altering genes. Concerns about equity, unintended consequences, and regulatory oversight challenge the notion of treatment, pushing us to reconsider who benefits from such advancements. Therefore, navigating the field of CRISPR ethics demands a careful, thoughtful approach that balances innovation with moral responsibility.
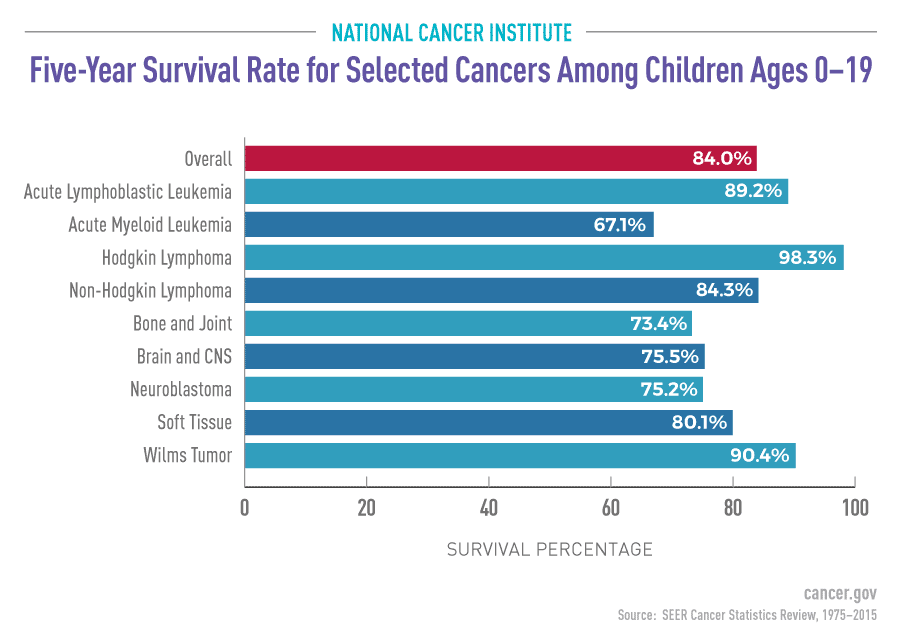
Pediatric Cancer Recurrence: AI Predicts Relapse Risks Accurately
Pediatric cancer recurrence remains a daunting challenge for many families, especially for those faced with pediatric gliomas, a type of brain tumor that can be both treatable and prone to relapse. Recent advancements in AI cancer prediction have opened new avenues for understanding the factors that contribute to cancer relapse risk. A cutting-edge study demonstrated that an AI tool analyzing longitudinal brain scans significantly outperformed traditional methods, providing more accurate forecasts of potential recurrences. The innovative approach of temporal learning in AI allows for the synthesis of multiple imaging results over time, enhancing the ability to discern subtle changes that could indicate a relapse. As research continues, the hope is that these enhanced predictive capabilities will lead to improved brain tumor treatment protocols and better outcomes for affected children.
Childhood cancer resurgence poses a significant problem, particularly with brain tumors like pediatric gliomas, which can be managed but still present a risk of returning. The integration of artificial intelligence in cancer prediction is transforming the landscape of medical diagnostics, allowing researchers to assess cancer relapse probability with unparalleled accuracy. By employing dynamic data analysis techniques that leverage the temporal aspect of patients’ imaging records, this innovative research enhances our understanding of relapse mechanisms. As we delve into the correlation between initial treatment success and subsequent monitoring, it’s crucial to explore how these AI-driven insights can refine therapeutic strategies and improve the management of pediatric cancer cases. Ultimately, the journey towards optimizing treatment outcomes hinges on our ability to harness technology effectively in the ongoing battle against recurrence.
The Importance of Early Detection in Pediatric Cancer Recurrence
Early detection of pediatric cancer recurrence is crucial for improving treatment outcomes and patient survival rates. Traditional follow-up methods, primarily relying on periodic scans, often leave both healthcare providers and families anxious about the patient’s prognosis. By harnessing advanced technologies like AI cancer prediction models, medical professionals can now have an early indication of potential relapse risk, enabling timely interventions that could be life-saving.
Children diagnosed with cancers like pediatric gliomas typically face a difficult journey that varies significantly based on the tumor’s characteristics. With the integration of AI tools that analyze multiple brain scans longitudinally, we can enhance the accuracy of detecting changes indicative of recurrence. This approach not only alleviates parental fear but also reduces the emotional toll on the children undergoing frequent and invasive imaging processes.
How AI is Transforming Pediatric Brain Tumor Treatment
AI’s role in transforming pediatric brain tumor treatment cannot be overstated. The ongoing research has shown that using temporal learning techniques allows for a more comprehensive analysis of brain scans, which can help predict pediatric cancer recurrence more accurately. By evaluating multiple scans over time, AI algorithms can discern subtle changes that might signify an increased risk of cancer relapse, something that single-scan analyses often miss.
Incorporating AI into standard brain tumor treatment protocols means that children can receive personalized care tailored to their specific risk profiles. With a prediction accuracy of 75-89 percent, thanks to the advanced temporal learning model, this innovation represents a significant leap from the traditional methods that offered only 50 percent reliability. These improvements offer hope not just for minimizing the burden of unnecessary imaging but also for refining therapeutic strategies for at-risk patients.
Understanding Cancer Relapse Risk Through Temporal Learning in AI
Cancer relapse risk is a significant concern for pediatric oncologists and families alike. With pediatric gliomas, the risk of recurrence varies, making it essential for healthcare professionals to predict outcomes with precision. Recent advancements in AI, particularly the deployment of temporal learning, allow the analysis of sequential MR scans rather than relying solely on isolated images. This methodology provides a richer dataset for the AI to interpret, leading to a more nuanced understanding of patient risks.
Temporal learning processes in AI can train models that not only recognize patterns in the patient’s imaging data but also relate those patterns back to potential recurrence scenarios. By understanding these dynamics, medical practitioners can better advise families on follow-up care protocols, reducing the need for frequent and possibly unnecessary scans for low-risk patients while ensuring that high-risk individuals are closely monitored and even pre-emptively treated.
The Role of Conventional Methods vs. AI in Cancer Recurrence Prediction
Conventional methods of predicting cancer recurrence typically rely on clinical judgment and periodic imaging, which can create inconsistencies and stress for families. Without a robust tool for timely prediction, patients might experience delays in treatment or unnecessary emotional strain due to the uncertainty surrounding their prognosis. In contrast, the emergence of AI tools specifically designed to predict pediatric cancer recurrence offers a revolutionary approach that can refine these processes.
By utilizing advanced AI algorithms trained on large datasets, researchers have found that these tools can outperform traditional methods by providing more accurate assessments of cancer relapse risk. This reliability could limit the frequency of imaging for patients deemed to be at lower risk while equipping healthcare providers with the insights needed to implement aggressive monitoring and intervention strategies for higher-risk children.
Innovations in Brain Tumor Research Insight for Families
For families navigating the complexities of pediatric brain tumors, understanding the forefront of research is vital. Advancements in AI-driven predictive models can offer them hope and clarity regarding their child’s condition. This innovation suggests that a more informed, data-driven approach to care can minimize anxiety about the future, allowing families to focus on recovery rather than uncertainties associated with potential cancer recurrence.
The promise of AI in brain tumor research not only pertains to developing tools for early detection but also extends to enhancing communication between families and healthcare providers. By providing tangible metrics and predictive assessments, families can engage more effectively in treatment decisions, ensuring that they are active participants in shaping their child’s medical journey.
The Future of Pediatric Cancer Care with AI Tools
Looking ahead, the integration of AI tools in pediatric cancer care heralds a new era of personalized medicine. As researchers explore the full potential of AI for predicting pediatric cancer recurrence, the hope is that clinical practices will evolve to incorporate these smart technologies seamlessly into routine care. This transition could mark a turning point in patient management strategies, promoting more proactive and tailored interventions.
Furthermore, as studies validate AI’s accuracy in predicting outcomes, we can expect systematic changes in how pediatric cancers are treated globally. This means potentially less invasive monitoring for low-risk patients and timely interventions for those at heightened risk, thereby facilitating a more effective overall treatment plan.
Advancing Imaging Techniques to Combat Cancer Relapse
Advancements in imaging techniques are crucial for an effective fight against pediatric cancer relapse. With the application of AI, especially through methods like temporal learning, healthcare providers can analyze a series of MR scans comprehensively. This robust approach yields deeper insights into how tumor remnants’ behavior over time might indicate a relapse, contributing significantly to patient outcomes by enabling more targeted interventions.
The evolution of imaging technology not only enhances the detection capabilities but also offers a more patient-friendly approach to monitoring outcomes in young children. Improved methodologies are essential to increase the likelihood of identifying worrisome changes early in the course of treatment, thereby providing clinicians a head start in potentially preventing a relapse through timely interventions.
AI-Powered Predictions Leading to Tailored Treatments
AI-powered predictions play a transformative role in tailoring treatments for pediatric cancer patients. By accurately predicting which patients are at risk for recurrence, oncologists can customize treatment plans that consider individual needs and risk profiles. This individualized approach may include decreased surveillance for low-risk families or more aggressive adjuvant therapies for those identified as high-risk.
Moreover, this targeted treatment approach promoted by AI technologies fosters an environment where pediatric patients experience less anxiety and a better quality of life. Families can focus on positive milestones in their child’s recovery journey rather than being overwhelmed with the ongoing threat of cancer relapse, ultimately leading to a more supportive and hopeful experience.
Understanding Pediatric Gliomas: Types and Treatments
Pediatric gliomas are classified into various types, depending on their grade and growth behavior. While many gliomas can be effectively treated with surgical intervention, they carry a significant risk of recurrence, highlighting the need for continuous monitoring. Understanding the nature of these tumors is critical for parents and caregivers in navigating treatment options and expectations.
Treatment modalities have evolved substantially, with combinations of surgery, radiation, and chemotherapy being deployed based on the tumor’s characteristics. However, with the introduction of AI in clinical settings, there are promising advancements in predicting outcomes and tailoring these approaches, maximally enhancing survival and quality of life for many children battling these tumors.
Frequently Asked Questions
How does AI improve predictions of pediatric cancer recurrence?
AI enhances the predictions of pediatric cancer recurrence by analyzing multiple brain scans over time utilizing a method called temporal learning. This approach identifies subtle changes in imaging that correlate with the risk of cancer relapse, providing a more accurate assessment than traditional single-scan methods.
What is the role of temporal learning in predicting pediatric gliomas recurrence?
Temporal learning plays a critical role in predicting pediatric gliomas recurrence by allowing AI models to learn from sequences of MR scans taken over time. This sequential analysis helps the model recognize trends and changes indicative of potential relapse, significantly improving prediction accuracy.
What are the risks associated with pediatric cancer relapse in gliomas?
The risks associated with pediatric cancer relapse in gliomas can be severe, leading to more complex treatment needs and adverse outcomes. Early prediction of cancer relapse risk using AI helps identify at-risk patients, potentially mitigating the impact of recurrence on their health.
How effective is AI in predicting cancer relapse risk compared to traditional methods?
AI has proven to be significantly more effective in predicting cancer relapse risk in pediatric patients than traditional methods. In recent studies, AI models achieved an accuracy of 75-89% using temporal learning, while traditional approaches based on single MR images had an accuracy around 50%, no better than random chance.
What implications does AI cancer prediction have for brain tumor treatment in children?
AI cancer prediction can transform brain tumor treatment in children by enabling more personalized care strategies. Enhanced prediction of recurrence risk allows for more tailored follow-up procedures and therapeutic interventions, ensuring higher-risk patients receive timely and appropriate treatment.
Can AI tools help reduce the stress of follow-up imaging in pediatric cancer patients?
Yes, AI tools can help reduce the stress associated with follow-up imaging in pediatric cancer patients by accurately identifying those at low risk for recurrence. This could potentially decrease the frequency of unnecessary imaging, alleviating some of the burden on patients and families.
What future developments are expected in AI and pediatric cancer recurrence prediction?
Future developments in AI and pediatric cancer recurrence prediction include further validation of temporal learning models across various clinical settings and the launch of clinical trials to assess the real-world effectiveness of AI-informed risk predictions in improving patient care.
| Key Point | Details |
|---|---|
| AI Tool for Prediction | An AI tool predicts relapse risk in pediatric cancer patients more accurately than traditional methods. |
| Study Focus | The study focuses on pediatric gliomas, which vary in recurrence risk and are usually treatable. |
| Temporal Learning | The use of temporal learning helps analyze multiple brain scans over time for better predictions. |
| Accuracy Improvement | AI model accuracy was found to be 75-89% compared to roughly 50% for single-image predictions. |
| Clinical Implications | The ultimate goal is to adjust imaging frequency and treatment based on predicted risk. |
Summary
Pediatric cancer recurrence is a serious concern that affects many families. Recent advancements in AI technology have shown promise in predicting the risk of recurrence in pediatric glioma patients with significantly better accuracy than traditional methods. This innovative approach not only aids in improving the predictive capabilities but also has the potential to transform patient care by allowing for more personalized treatment strategies.